Salt and your IQ
Iodized salt has been on the market for decades, but do you know why it is so important for you? Iodine deficiency is one of the most common causes of preventable mental retardation worldwide. Moderate to severe iodine deficiency is associated with reductions of 13.5 points in mean intelligence quotient (IQ).
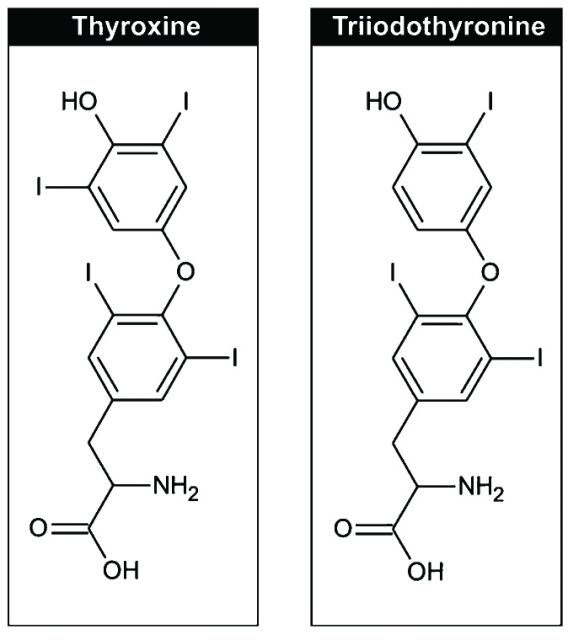
Iodine is an important component of thyroid hormones, which regulate numerous physiological processes from growth to neurological development and reproductive function. The thyroid gland secretes the hormones triiodothyronine (T3) and thyroxine (T4). T3 is produced from T4 by the deiodinase enzyme. The chemical structures of T3 and T4 are schematized in Figure 1.
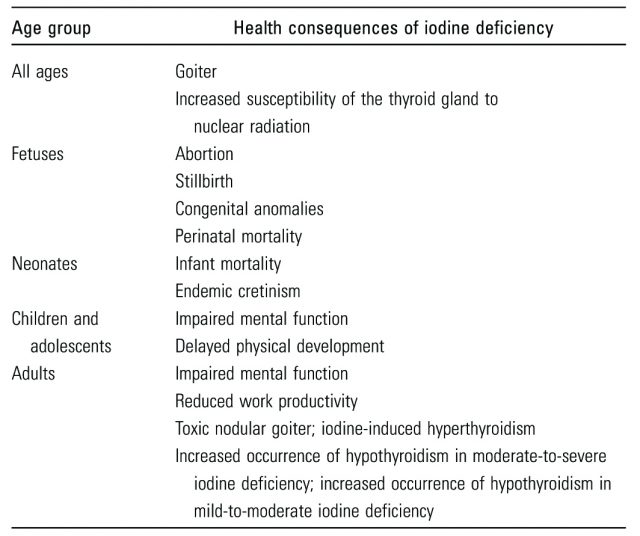
The range of disorders associated with iodine deficiency has been termed Iodine Deficiency Disorders (IDD) and affect almost two billion people worldwide. Table 1 summarizes IDD by age group. Typically, iodine deficiency causes goiter, which is an enlargement of the thyroid. A more severe consequence of iodine deficiency is cretinism. Cretinism results in mental retardation and additional developmental defects, including deaf-mutism, short stature, and neuromuscular abnormalities.
Due to the important health implications for iodine deficiency, the Iodine Global Network (IGN) – formerly known as the International Council For Control of Iodine Deficiency Disorders (ICCIDD) – was established in 1985. The sole purpose of IGN is to achieve optimal iodine nutrition worldwide.
Moreover, the National Institute of Health (NIH), in collaboration with global partners, created the Biomarkers of Nutrition for Development (BOND) Program. The program aims to discover, develop, and implement reliable biomarkers to assess nutrient exposure, status, function, and effect. Iodine is one of the micronutrients in the scope of the BOND Program. Recently, the organization published a review describing iodine biology and the current available biomarkers of iodine 1. This article summarizes the main aspects of the review.
Before introducing iodine biomarkers, the BOND review provides and overview of issues pertaining to iodine exposure, including dietary assessment of iodine intake and household coverage of iodized salt, since they are crucial for the iodine status of populations.
In contrast to other diseases, iodine deficiency is not related to the level of development in a country. Instead, iodine deficiency is related to geography; countries with low iodine content in their soil have low iodine foods. Therefore, individuals who depend on food sources grown in iodine deficient soils become iodine deficient.
Iodine is an essential nutrient, i.e., it has to be obtained from dietary sources. The World Health Organization (WHO) recommendations2 for iodine daily intake are: age 0-5 years, 90 micrograms (μg); age 6-12 years, 120 μg; age >12 years, 150 μg; and pregnant and lactating women, 250 μg. While iodine is present at low levels in most foods, some foods contain higher levels of iodine. Foods such as milk and milk products are sources of iodine. In addition, saltwater fish and other types of seafood have relatively high iodine content because they concentrate iodine from seawater.
On the other hand, some foods inhibit iodine metabolism. These substances are known as goitrogens and they have various mechanisms of action. For instance, the flavonoids present in soy impair thyroid peroxidase activity, which is crucial for thyroid hormone production. However, broccoli and other cruciferous vegetables contain glucosinolates that compete with iodine for thyroidal uptake.
Overall, the amount of iodine ingested in the diet is normally not enough to meet our body’s iodine requirements. A cheap and easy way to increase the intake of iodine in a given population is to implement salt iodization. It is estimated that every dollar invested in salt iodization returns US$30 in benefits 3. Consequently, universal salt iodization is currently the main strategy to eradicate IDD globally.
Household iodized salt coverage is an indicator of the progress of salt iodization strategies across countries. The threshold defining a successful iodization program is coverage of 90% of households using adequately iodized salt. Salt is considered adequately iodized when it contains at least 15 mg/kg (15 ppm) of iodine. Nowadays, around 70% of the population worldwide has access to adequately iodized salt.
The clinical biomarkers for iodine deficiency described in the review published by the BOND Program include (Rohner et al. 2014):
-
urinary iodine concentration (UIC)
-
thyroid-stimulating hormone (TSH)
-
thyroglobulin
-
T4 and T3, and
-
goiter.
To date, the UIC is the most reliable biomarker to assess the iodine status of populations. Because 90% of dietary iodine eventually appears in the urine, UIC is an excellent indicator of recent iodine intake. UIC is normally measured in spot urine specimens and reported as the median concentration (μg/L) in the population. UIC is measured at a population level as it varies between individuals on a daily basis, depending on their recent iodine intake. There is also diurnal variation in UIC, with concentrations generally increasing over the course of the day. Thus, UIC needs sufficiently large sample size to even out inter- and intra-individual variation and must be performed on a population level.
When estimating the iodine status of the population, school-aged children, pregnant and lactating women, and women of reproductive age, are targeted. It is believed that if these target groups present optimal iodine nutrition, the entire population will. The acceptable median UIC cutoffs for adequate iodine intake differ between these target groups. For example, median UIC levels of 100-299 μg/L in school-age children and 150-249 μg/L in pregnant women are deemed adequate. In lactating women, the adequate iodine intake cutoff is lower (i.e., ≥100 μg/L), as iodine is also excreted in breast milk. A low median UIC value in these target groups suggests a population is at risk of developing IDD.
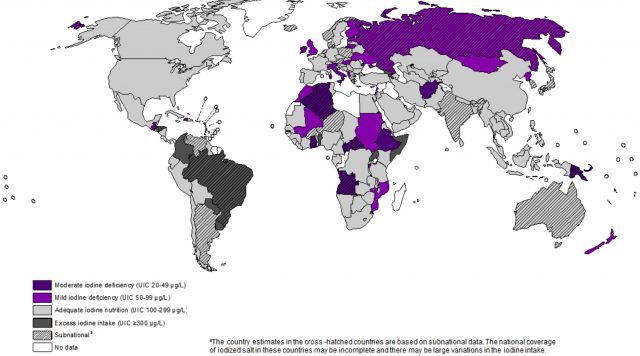
Despite efforts to eradicate iodine deficiency, mild to moderate iodine deficiency still affects 32 countries, many of them in the industrialized world. Figure 2 shows the global distribution of iodine deficiency based on median UIC in 2011. A more recent interactive map of the iodine status of the population worldwide can be found here (IGN).
Paradoxically, attention must also be paid to excess iodine intake, since it also causes adverse health effects. Countries like Brazil and Somalia present excessive iodine intake, defined as median UIC >300 μg/L.
Finally, when implementing salt iodization programs it is important not to encourage excess salt consumption. High salt consumption contributes to high blood pressure and increases the risk of heart disease and stroke. WHO recommends that adults consume less than 5 g (just under a teaspoon) of salt per day (WHO). The concentration of iodine added to salt goes hand in hand with salt consumption. The less salt the population consumes, the higher the iodine concentration should be in salt to meet iodine requirements.
After reading this article I hope that the next time you buy salt, you make sure it is iodized. But remember not to add too much salt to your food! The health problems associated to excessive salt intake may be discussed in a future Mapping Ignorance article.
References
- Rohner F, Zimmermann M, Jooste P, Pandav C, Caldwell K, Raghavan R, Raiten DJ. Biomarkers of nutrition for development-iodine review. The Journal of Nutrition. 2014, 144(8):1322S-1342S ↩
- World Health Organization. Salt reduction Fact Sheet. 2011, N.393. ↩
- ICCIDD. Investing in the future: a united call to action on vitamin and mineral deficiencies.IDD Newsletter. 2009, 33(3):14-16 ↩
3 comments
I have been reading your article in mapping ignorance about iodadazed salt consumption and IQ.
I like it very much, because it gives a very good general idea of the question. Nevertheless in my opinion, in countries like Spain, where iodine supplementation during pregnancy is a general practice, the problem could be another and it has already been studied: the risk related to the high supplementation for the mother and for the child.
There a few good articles related to this issue that has been studied in the INMA (INfancia and Medio Ambiente) prospective project.
Hugs / abrazos / besarkadas.
[…] Los déficits en algunos nutrientes pueden tener efectos sobre la salud. Si no tomas suficiente iodo, por ejemplo, eres significativamente más tonto. Y es facilísimo (y muy barato) evitar que ocurra. Laura Cascales en Salt and your IQ […]
Good article, i didn’t knew about importance of iodine on our health. I will have it on count for my diet.