Novel strategies to selectively reduce pain
Novel strategies to selectively reduce pain
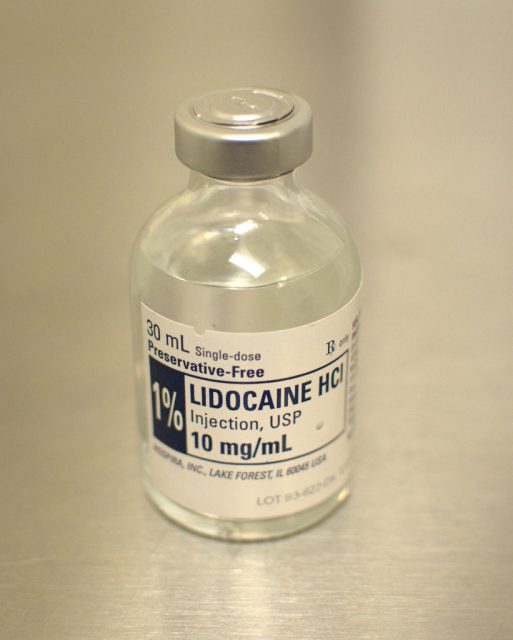
A recurrent problem with pain is the absence of therapeutic strategies to selectively block the nociceptors (neurons responsible to detect painful stimuli) that need to be targeted for a particular indication. Things get even worse if we take into account that some molecules used for pain management do affect other, more general physiological processes. Local anaesthetics, for instance, are a tool widely used by clinicians to block pain without affecting consciousness. The compound of choice is injected into the region where the pain is expected to be experienced. The problem with these molecules relies on the fact that besides pain, there is a concomitant abolition of the motor and autonomic functions. The reason is that these anaesthetics -which includes lidocaine and derivatives- block all types of sodium channels expressed in peripheral neurons. At high concentrations, they can even affect the cardiac muscle leading to cardiovascular toxicity issues, mainly because sodium channels are key components expressed on excitable cells with the role to propagate action potentials (a process already explained in more detailed on previous MI posts). The reason for such unspecific action relies on their permeability profile; these compounds can move across the plasma membrane due to their lipophilic chemistry and get into the cytoplasm blocking the sodium channels intracellularly. Thus, if one could figure out a way to make the anaesthetic impermeable and somehow let it get only into the targeted nociceptors, it could prevent all these undesirable side effects.
This is indeed the strategy the group of Professor Clifford J Woolf from the Harvard Medical School has been trying to make work for some years now. The impermeable lidocaine derivative is called QX-314 and is permanently charged by a quaternary nitrogen, preventing it from passing through the cell membrane. The first problem solved but, how to introduce the molecule only into selected populations of nociceptors? If you are familiar with my previous posts in MI, you may have heard about the nociceptive ion channel TRPV1, critical to detect and initiate pain-related sensory processes. Because TRPV1 is only expressed in these sensory neurons and it has been shown to have a large conducting pathway (pore), in their first attempt they co-injected both QX-314 and capsaicin into rat hind paws or sciatic nerve as a way to specifically activate nociceptors expressing TRPV1. Capsaicin is a potent TRPV1 agonist found in chilli peppers that activates the ion channel. The local anaesthetic gets into the neurons blocking the conduction of the pain information to the brain (by blocking the sodium channels). Injections resulted in a diminished response to both mechanical or thermal painful stimuli, corroborating the suitability of the approach because no motor deficit was observed in the rats 1.
The problem is capsaicin itself: a very painful stimulus that produces a burning pain sensation. In addition, application must be prolonged (as it takes minutes for QX-314 to get into nociceptors), so it does not make much sense trying to prevent pain producing pain on the patient. Therefore, an alternative had to be found taking also into account formulation issues (ideally a lipophilic agonist). Serendipitously, a different study found that lidocaine applied at clinical concentrations (30 mM) was itself a TRPV1 agonist 2, making it the ideal TRPV1 activator as there is a large body of toxicological information accumulated through the years. Next step would be to find the right proportion of both local anaesthetics to prevent as much as possible the lidocaine-related broad action with enough QX-314 to achieve sustained pain relief.
Again, rats were co-injected on the sciatic nerve using different concentrations of both molecules to optimize the ratio between “pain-specific” and “non-selective” effects. Although we are not going into much detail here, they (surprisingly) found that co-application of 2% lidocaine (it can be used at concentrations up to 4% clinically) and 0.5% QX-314 (no available clinical data), resulted in 1 h of broad pain, motor and autonomic block but followed by 9 h of a pain-specific phase. Although studies in humans should confirm the lack of QX-314-mediated toxicity, this novel approach where ion channels are used as a “drug-delivery platform” could be proven clinically useful. In this particular case, the application is tailored for pain management but perhaps a similar strategy could be used to alleviate other conditions. An even more futuristic possibility may involve the artificial design and synthesis of artificial ion channels which could be inserted or expressed on targeted cells (that may be the most difficult step, indeed) to deliver therapeutic molecules to them. There is some work being done to this respect already 3, although again one should not be too optimistic about these things being available anytime soon.
References
- Binshtok AM, Bean BP, Woolf CJ. Inhibition of nociceptors by TRPV1-mediated entry of impermeant sodium channel blockers. Nature. 2007 Oct 4;449(7162):607-10. doi: 10.1038/nature06191. ↩
- Roberson DP, Binshtok AM, Blasl F, Bean BP, Woolf CJ. Targeting of sodium channel blockers into nociceptors to produce long-duration analgesia: a systematic study and review. Br J Pharmacol. 2011 Sep;164(1):48-58. doi: 10.1111/j.1476-5381.2011.01391.x. Review. ↩
- Kumar YP, Das RN, Kumar S, Schütte OM, Steinem C, Dash J. Triazole-tailored guanosine dinucleosides as biomimetic ion channels to modulate transmembrane potential. Chemistry. 2014 Mar 10;20(11):3023-8. Erratum in: Chemistry. 2014 Mar 24;20(13):3547. PubMed PMID: 24677317. ↩
3 comments
[…] Los anestésicos tienen muchos efectos sesundarios indeseados. Lo suyo sería un calmante del dolor que actuase justo donde hace falta. Sergio Laínez en Novel strategies to selectively reduce pain […]
Great post!
Do we know if this compound will be soonly ready to be used on the market?
Thanks for your question, Franck…a good one, indeed.
This is always the tricky part. The path to launch a new molecule to market is always long, difficult and fairly expensive, to be honest. I addition, you always need support from a large companies with both the clinical experience and financial resources to move it forward. Even though this is a lidocaine derivative, which is an already commercially available anaesthetic, a big deal of clinical studies (including toxicology) will have to happen for QX-314 to be approved as a medicament. Just so that you know, the original Nature paper was published back in 2007, so 10 years have passed already and the molecule is still in pre-clinical stage, so I guess we will have to wait still a bit before we can use it, for instance on the dentist…which is the most obvious and straightforward application that may come to mind.