Heterogeneous sorroundings are critical in the analysis of nerve ablation for treating chronic pains
Chronic pain is one of the most common problems of advanced age. Even though the combination of physical therapy and analgesics such as nonsteroidal anti-inflammatory drugs is effective in chronic pain treatments, it only confers short-term benefits. On the other hand, it could be quite expensive and may have significant adverse side effects.
Effective, lasting and cheaper alternatives are, therefore, considered, as the primary goal of the physicians responsible for the management of chronic pain is to find long-term solutions rather than short-lived interventions. Consequently, nonsurgical minimally invasive options for treating chronic pain have surged during the past decades, all of them focused on targeting nerves transmitting pain signals. Cryoablation (use of extreme cold), various laser therapies, high temperature radiofrequency, and chemical neurolysis, such as alcohol or phenol, are some of these options.
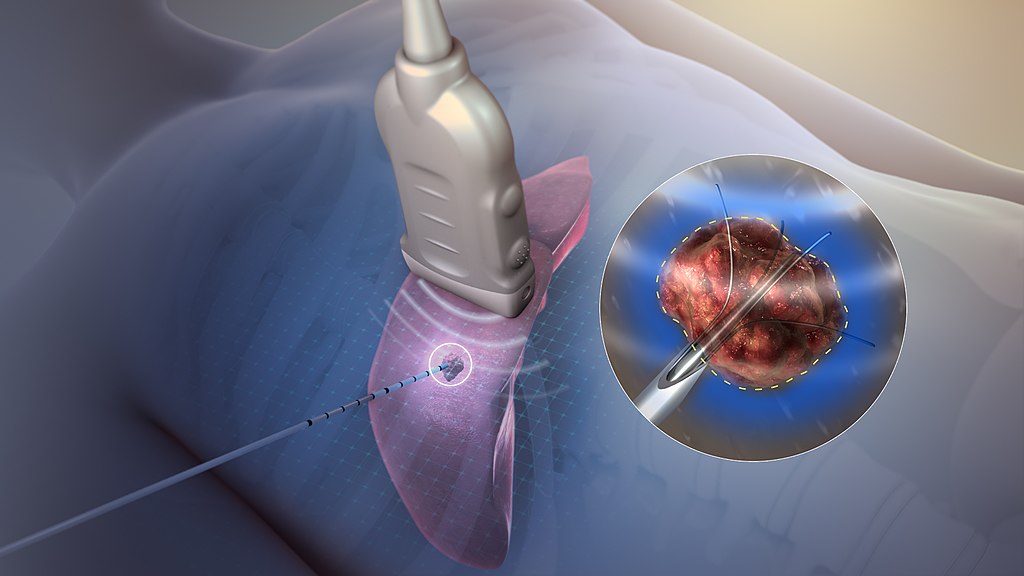
Among these nonsurgical modalities, radiofrequency ablation (RFA) offers the advantage of being precise, reproducible, cheap and effective to a great extent. In radiofrequency ablation (RFA) part of the electrical conduction system of a dysfunctional tissue is ablated using the heat generated from medium frequency alternating current. RFA is generally conducted in the outpatient setting, using either local anesthetics or conscious sedation anesthesia. When it is delivered via catheter, it is called radiofrequency catheter ablation. The application of RFA is well tested for treating various tumors in liver, lung, kidney, bones, prostate, and breast.
During RFA, a high frequency alternating current in the frequency range of 500 kHz is applied in the vicinity of a nerve via an electrode, leading to neurodestructive thermocoagulation, thereby degrading its ability to conduct pain signals. The lesion produced due to the resistive heating during the RFA procedure may give pain relief for 12-18 months or longer, with minimal side effects and associated complications. Since the largest area of thermal lesion is produced along the axis of the electrode, the electrode is precisely placed parallel to the target nerve so as to maximize the damage to the adjacent nerve fibers.
Several patient specific clinical studies of RFA in treating chronic pain of bones have already been performed and reported in the literature, though questions regarding anatomical targets, selection criteria, and evidence for effectiveness, are still open.
Now, Sundeep Singh and Roderick Melnik 1have evaluated the effects of target nerve distance from the bone tissue during continuous RFA for chronic pain relief.
Numerical modeling and simulations provide a powerful tool to predict such important characteristics as the temperature distribution and lesion volume during RFA. They give a quick, convenient and inexpensive a priori information during the treatment planning stage of RFA to medical practitioners. The present study is one of the first of its kind, focusing on the mathematical modeling of RFA in treating chronic pain within bones. As a result, the effect of target nerve distance from the bone on the efficacy of the continuous RFA procedure is quantified.
The authors consider a generalized three-dimensional heterogeneous computational model comprising muscle,bone and target nerve. The continuous RFA is performed through a monopolar needle electrode placed parallel to the target nerve. Finally, the electric field and temperature distributions as well as the lesion volume attained during continuous RFA are obtained via a finite-element-based coupled thermo-electric analysis.
The researchers find that there prevails a strong dependence of the distance between the target nerve and the bone on the outcomes of RFA. The nerve ablation volume decreases for the target nerve located closer to the bone and vice versa. Consequently, the effect of the heterogeneous surrounding in the analysis of nerve ablation for treating chronic pains is found to be critical and, therefore, conclusions from oversimplified studies based on the homogeneous surrounding assumption should not be considered.
Author: César Tomé López is a science writer and the editor of Mapping Ignorance
Disclaimer: Parts of this article may be copied verbatim or almost verbatim from the referenced research paper.
References
- Sundeep Singh and Roderick Melnik (2019) Radiofrequency Ablation for Treating Chronic Pain of Bones: Effects of Nerve Locations. In: Rojas I., Valenzuela O., Rojas F., Ortuño F. (eds) Bioinformatics and Biomedical Engineering. IWBBIO 2019. Lecture Notes in Computer Science, vol 11466. Springer, Cham doi: 10.1007/978-3-030-17935-9_38 ↩