Health-related quality of life in chronic obstructive pulmonary disease patients
Health-related quality of life in chronic obstructive pulmonary disease patients
Chronic diseases are already having and will continue to have not only profound economic, social and individual consequences but also a major impact on the use of health resources and design of new care processes. Chronic obstructive pulmonary disease (COPD) is a case on point.
COPD is airflow limitation caused by an inflammatory response to inhaled toxins, often cigarette smoke. Alpha-1 antitrypsin deficiency and various occupational exposures are less common causes in non-smokers. Symptoms are productive cough and dyspnoea that develop over years; common signs include decreased breath sounds, prolonged expiratory phase of respiration, and wheezing 1. COPD is understood as a complex heterogeneous multisystem disease, with varying levels of progression and activity in different patients. This complexity makes necessary to devise tools to help us evaluate as broadly and comprehensively as possible the disease.
A metric called health-related quality of life (HRQoL) gives an overall view of the general clinical condition of a patient. It is considered an important outcome in itself in many diseases. Even though HRQoL is commonly used as a predictor of other outcomes such as mortality in COPD patients, it should be used more frequently in daily clinical practice. Actually, HRQoL is very often assessed in clinical trials but its use in routine clinical practice and the impact of this use on practice has not been thoroughly studied.
Many studies have identified various different factors associated with HRQoL in COPD patients; however, what has not been thoroughly studied is whether these factors maintain their influence over time. It is noteworthy that these previous cross-sectional studies tend to have only assessed HRQoL at the start of the study and take it for granted that the data were normally distributed.
Now, a team of researchers has identified 2 variables associated with HRQoL, in a real-life scenario, without any kind of established intervention, and assessed whether these variables initially associated with HRQoL continue to have an influence in the medium-term during follow-up. They found that a normal distribution is not the best fit.
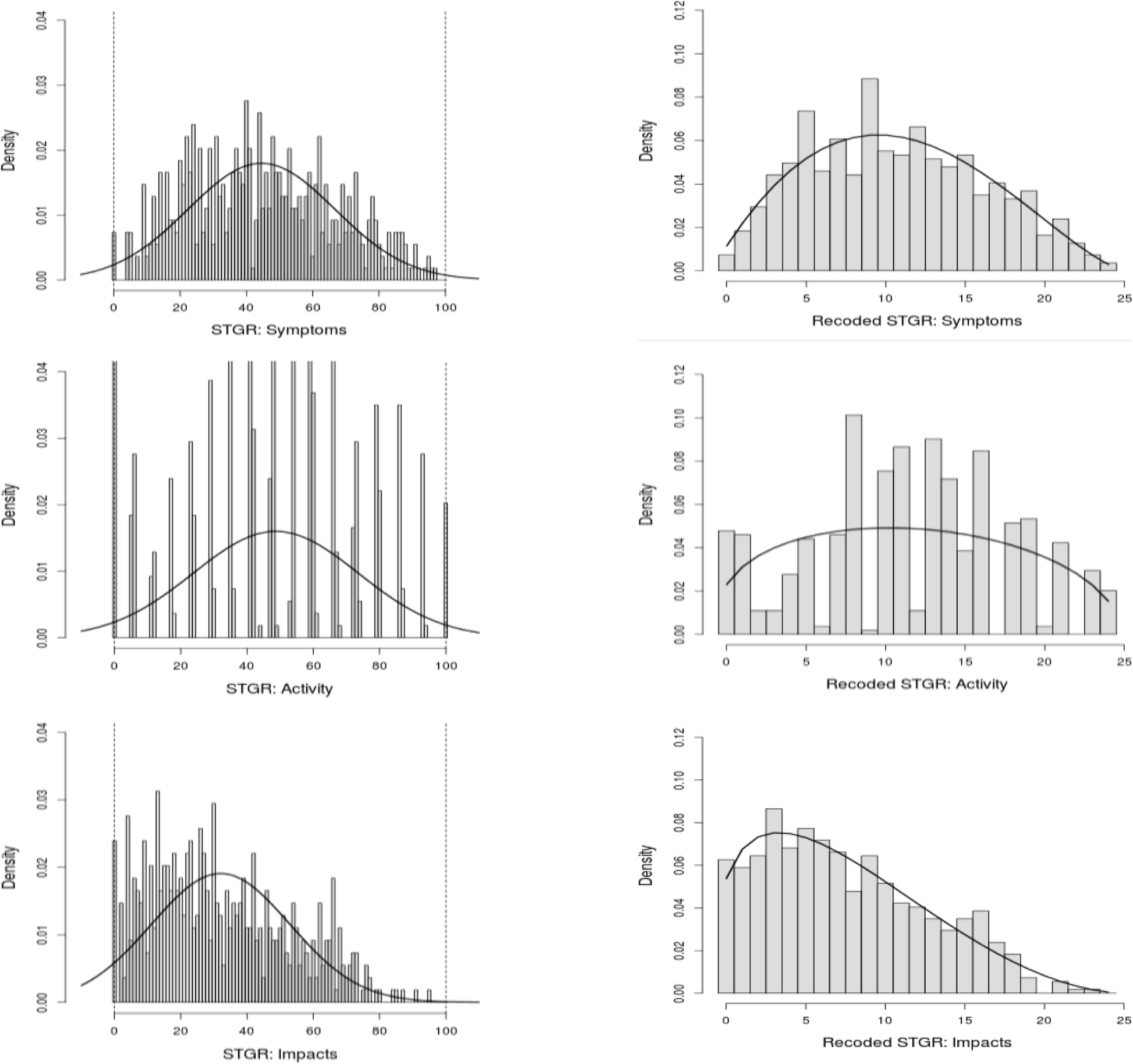
distribution (left); and recoded to an ordinal scale from 0 to 25 and their fit to the beta-binomial distribution (right)
The researchers found that among COPD patients, HRQoL was associated with the same variables throughout the study period, most importantly two key modifiable factors: physical activity and hospitalizations for exacerbation. They also show that a beta-binomial distribution reproduce much better the results than the expected normal one.
Author: César Tomé López is a science writer and the editor of Mapping Ignorance
Disclaimer: Parts of this article may be copied verbatim or almost verbatim from the referenced research paper.
References
- Robert A. Wise (2020) Chronic Obstructive Pulmonary Disease Merck Manual Professional Version ↩
- Esteban, C., Arostegui, I., Aramburu, A. Javier Moraza, Josu Najera-Zuloaga, Myriam Aburto, Susana Aizpiri, Leyre Chasco & José M. Quintana (2020) Predictive factors over time of health-related quality of life in COPD patients. Respir Res. doi: 10.1186/s12931-020-01395-z ↩