Chasing painful channels
Chasing painful channels
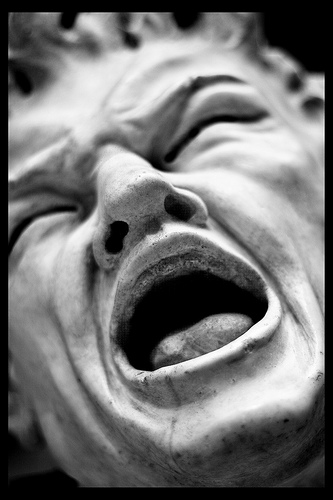
Most people have experienced how does it feel when dipping a finger into boiling water or swallowing while having tonsil inflammation. Pain may be annoying, but it is an essential protective mechanism because it warns us against potential tissue damage. This necessary role in survival is illustrated by the shortened life expectancy seen in individuals suffering from rare diseases such as congenital insentivity to pain. Patients with this disorder often die prematurely as a consequence of accidental injuries because they don’t know what pain means.
Generally speaking, pain can be classified into three main types taking into account the association between painful stimuli and the sensation that it evokes. Acute pain originates after the application of a brief painful stimulus that can be of physical (hitting a finger with a hammer) or chemical (step into a nettle) nature. Inflammatory pain appears as a consequence of infection or sustained tissue damage involving the release of inflammatory mediators and immune cells. These types of pain are of relevance for the survival of the organism, as they will result in protective behaviour aiming to minimise harm. The third one is neuropathic pain and is caused by injury to nerves, including both peripheral and central ones. This type of pain has no recognizable survival function and is, therefore an aberrant neurological response from the organism.
Both acute and inflammatory pain have been extensively studied in the last decades at the molecular and cellular level, but still little is known about the molecular mechanisms explaining neuropathic pain and it has only been recently when some progress has been made so far. That means that basic and clinical research has helped to identify a plethora of molecules, including proteins, linked to the former pain modalities, but we largely lack information about proteins involved in neuropathic pain mechanisms, at least in peripheral nervous system, which detect and initiates pain responses.
But why worry about neuropathic pain? Because it is of clinical relevance as often (more than we would like to) becomes chronic, impairing quality of life. It is a symptom associated with conditions such as arthritis, diabetes, postherpetic neuralgia or tumors, among others and typically only 30% of patients respond to even the gold standard US Food and Drug Administration (FDA) approved treatments1.
In an attempt to identify molecular players important to the development of neuropathic pain, the lab from Peter McNaughton in Cambridge (UK) took advantage of transgenic-engineered mice to study the potential role in neuropathic pain of a previously known ion channel, hyperpolarization-activated cyclic nucleotide ion channel isoform 2 (known as HCN2)2. HCN channels comprise four different members named 1 to 4 (HCN1-HCN4) and are quite unique as they are gated (meaning activated) in response to hyperpolarizing membrane voltage potentials. Accordingly, they play an important role as pacemaker channels contributing to modulate the action potential firing (spiky responses from neurons) in the central nervous system (CNS) and more important, to the cardiac heartbeat, mediated by HCN4 expressed in sinoatrial node cells (mice lacking HCN4 prematurely die in embryonic stage).

Because information related to pain is signalled by the frequency of action potentials in the peripheral neurons (called nociceptors) and the frequency of firing is higher when the painful stimulus is stronger, the working hypothesis from the authors was that HCN2 (previously known to be expressed in nociceptors) could account to changes in firing frequency and hence could be relevant to conduct information related to pain to CNS.
To test the hypothesis, the lab developed a knockout mouse where the HCN2 gene was deleted leading to a complete absence of the protein in the mouse. Unfortunately, the crucial role of the ion channel in CNS made impossible to study its function in vivo as these animals are severely affected, developing ataxia and epilepsy. For this reason, a second approach consisting of developing a conditional knockout mouse had to be taken. Because the same protein may have different role in different types of cells, in a conditional knockout, the absence of the protein only takes place in the cells under study (in our case, nociceptors), without affecting the expression of the same protein in the remaining cells of the mouse. This way, we can specifically disclose the action of the protein exclusively in those cells. Mice in which HCN2 deletion was restricted to a subset of nociceptors didn’t show any behavioural abnormality being therefore suitable to continue the study.
In a first set of in vitro experiments, the researchers collected the peripheral neurons expressing the HCN2 channel from the mouse and plated them in a petri dish. Because neuropathic pain cannot be tested in isolated neurons, the researchers treated them with the well-known inflammatory mediator prostaglandin E2 (PGE2) to successfully confirm an increase in their frequency of action potential firing. The same experiment was performed in the neurons from the mice where HCN2 was deleted, where the increase in firing was absent, indicating that HCN2 is at least important to conduct information regarding inflammatory pain. The results indicated that HCN2 present in nociceptors is involved in “sending” information about pain to higher centres in the brain. Nevertheless, this only holds true in “artificial” conditions as these neurons where plated in a plastic dish. What would happen in the mouse alive when applying a neuropathic pain model?
The next (and fundamental) step was, therefore to perform an in vivo experiment where the authors have to “emulate” a situation in which the mouse develops neuropathic pain. There are several ways to do that, but they chose a model called chronic constriction injury (CCI) where the sciatic nerve of the mice is exposed and compressed by applying a surgical suture (literally, doing a knot in the nerve). The surgery was done in both the wild-type mice (expressing HCN2) and the formerly mentioned conditional knockout where HCN2 was deleted from the subset of peripheral neurons. As expected (this is when researches say Hooray!), the mice expressing the channel showed all the classic symptoms that a patient with a neuropathy would show, while the mice not expressing the channel where happy and showing no behaviour associated with pain. In addition to that experiment, pharmacological block of the HCN2 channel injected into the wild-type mice (expressing HCN2) abolished neuropathic pain too, strengthening the result.
In view of the results, the authors propose that an inflammatory mediator released at the site of nerve injury, modify HCN2 in a way that result in an increased action potential firing frequency. This would be the starting event leading to neuropathic pain.
Obviously, the study raises questions such as: Why is the subset of peripheral nociceptors where HCN2 is deleted (remember our conditional knockout mice) crucial in neuropathic pain, given that the ion channel is also expressed in other subset of nociceptors as well? How many inflammatory mediators are capable of initiating the process and more important, is HCN2 activity important once neuropathic pain has been established, or is just a triggering factor followed by another cascade of events which may, in turn lead to the chronic nature of neuropathic pain? This is how research works; one answer is followed by a bunch of new fascinating questions.