Fight suicide!

Suicide is one of the worst health and social problems in the modern world. Hundreds of millions of persons experience suicidal thoughts every year and between 10 and 20 millions went on to attempt suicide. In Spain, although the average risk is lower than in Northern countries, almost 4.000 persons die every year by their own hands. There is no quick fix available for suicidal ideation. Usual treatments include antidepressants and some antipsychotic medications but these drugs are slow to act and can take one month or more to kick in and they are not always effective. Thus, a pharmacological solution for acute treatment of possible suicides is greatly needed. 90% of suicides are in people with clinically diagnosable psychiatric disorders; anxiety, depression, impulsivity and alcohol abuse are major risk factors and thus psychopharmacology is probably the only way. Tragically, research on suicidal behavior is an important and neglected topic, and many clinicians, organizations, and industry sponsors are reluctant to engage.
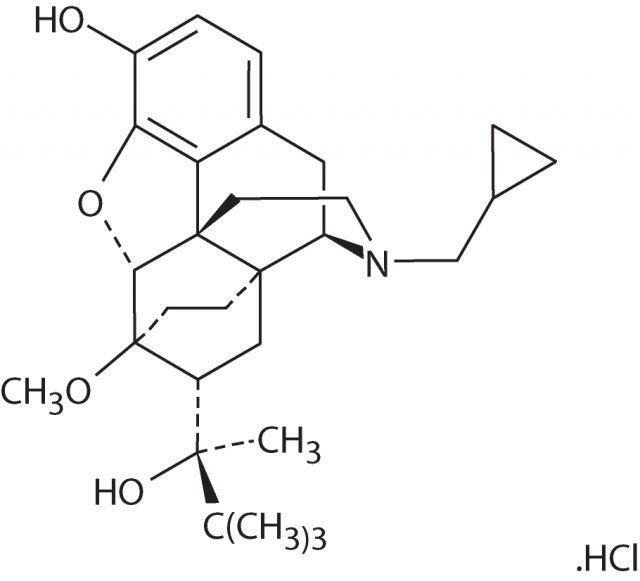
Recent investigations are considering the possibility of using «safe opioids» for the treatment of depression, as well as the chronic psychological pain that often acts a precursor of suicidal ideation 1. Buprenorphine, a partial agonist at µ-opioid receptors is one of these safe opioids whereas the analgesic effects are kept and the lethal (respiratory depression) risks are minimized. Buprenorphine shows less euphoria and physical dependence, lower potential for misuse, a ceiling on effects and a relatively mild withdrawal profile than other opioids.
Opioids are part of the natural chemicals in the brain. They are released to relieve pain and seem to be involved in psychological pain, the feeling you have when you lose a loved one. Buprenorphine is already clinically used to treat heroin addiction and has a good safety and efficacy record. It is characterized as «sticky» because of its capacity to latch onto the opioid receptors and block other substances from taking effect. So if someone was taking buprenorphine and decided to consume heroin, for example, the buprenorphine would prevent the heroin from getting him high.
Jaak Panksepp, a researcher from Washington State University spearheaded a clinical trial of buprenorphine in suicidal individuals 2. His group recruited 62 people thought to be severely suicidal (almost half of whom had attempted suicide) and 40 of them received very low doses of buprenorphine whereas the remaining 22 took a placebo (a 2:1 ratio). The authors tested the efficacy and safety of very low dosages of sublingual buprenorphine as a time-limited treatment for severe suicidal ideations. They did a multisite randomized double-blind placebo-controlled trial of ultra-low-dose sublingual buprenorphine as an adjunctive treatment. A psychiatric questionnaire, the Beck Scale for Suicide Ideation, was passed at the start of the trial showed an average of 20 points, a measurement severe enough to warrant hospitalization. It was also passed at the end of each of 4 weeks of treatment.
Readings fell by 6 points on average after a week for the buprenorphine patients, going down nearly 10 points after a month. This level already might not necessarily call for hospitalization. The placebo group also showed a smaller improvement after two weeks but this went away after a month. In fact, the placebo effect has been suggested that can be explained precisely by the release of opioids in the brain just for being in a healing medical atmosphere. No withdrawal symptoms were reported after treatment discontinuation at the end of the trial.
Panksepp considers that the fast effect could be even accelerated with higher doses and although there are risks with opioids analgesics, buprenorphine is not as problematic as others, such as ketamine, than can cause agitation, confusion, and psychosis although it is on the World Health Organization’s List of Essential Medicines, the most important medications needed in a basic health system. Nevertheless, opioids have a bad reputation for the treatment of depression. They were widely prescribed from the 1850s to the 1950s but they were addictive and overdoses could be fatal. Modern antidepressants replaced them.
Additional larger studies are necessary before it is safe to start recommending buprenorphine for treating suicidal depression. We need to establish the efficacy, safety, dosing, and appropriate patient populations for this experimental treatment. However, the fact that buprenorphine is already prescribed with good results for opiate addiction and the absence of available options for suicidal behavior suggest that for the first time something valuable to fight this psychiatric epidemic may be on the way.
References
- Locklear M (2016) Drug quickly quells suicidal thoughts. New Scientist 3059: 12. ↩
- Yovell Y, Bar G, Mashiah M, Baruch Y, Briskman I, Asherov J, Lotan A, Rigbi A, Panksepp J (2015) Ultra-Low-Dose Buprenorphine as a Time-Limited Treatment for Severe Suicidal Ideation: A Randomized Controlled Trial. Am J Psychiatry DOI: 10.1176/appi.ajp.2015.15040535 ↩