You have to learn how to die
…if you want to want to be alive.
The rock band Wilco already said it back in 2002 when they released the much-acclaimed album Yankee Hotel Foxtrot. This simple statement found in one of the songs of that LP was able to summarise the paradoxical essence of life: death. But leaving any philosophical meaning aside, lets focus on the biological fact. Maybe they were actually singing about apoptosis, the process through which cells commit suicide to ensure a correct functioning of eukariotic organisms.
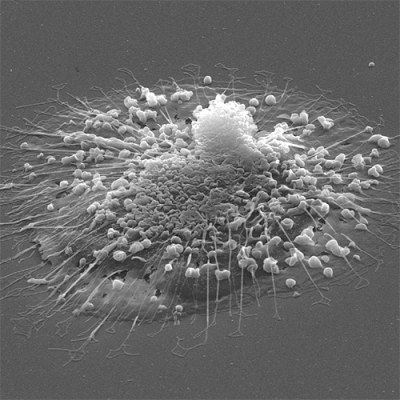
Cell death is so tightly regulated in our body that deficiencies in this mechanism are a major cause of cancer. Indeed, mutations affecting the function of genes that regulate apoptosis result in uncontrolled cell growth, ultimately leading to the formation of tumours. However, in normal conditions apoptosis occurs between 50 and 70 billion times per day to remove dysfunctional cells throughout our body. It is an essential process for the development of organs and systems, in normal cell homeostasis and in the defence against pathogens.
This is all very well, one might think, as apoptosis has been known for decades, widely studied and thoroughly characterised. However, only a few months ago one of the most surprising findings of the year, published in Nature, has put forward this biological process as the target of a drug withdrawn from the market after being found highly toxic in humans.
The story of Trovan, the market name of the antibiotic trovofloxacin, is not one without controversy. The drug was developed as a promising and highly effective antibiotic from the family of the commonly used quinolones. Prior to its release, the drug became sadly famous after allegedly causing death or severe malformations in children during the 1996 meningitis epidemic in Nigeria. This episode, that raised an intense public debate on the ethics behind clinical trials in developing countries, was settled with US$75 millioncompensation for the families. Besides, this caused great distrust of Western medicine amongst families in northern Nigeria and was one of the factors that led many to refuse letting their children be vaccinated against polio, which still is a prevalent disease in the area. Trovan was later found to be toxic for the liver and was withdrawn from the market or restricted to very specific applications in 1999.
Some few years later, on the other side of the world a lab was studying pannexins, a type of membrane proteins that act as channels for the release of the energy-carrying molecule ATP. To find inhibitors for these channels the researchers from Virginia (US) used a library of more than 1000 different bioactive compounds, including the infamous trovafloxacin. The surprise came when the drug was found to be a highly potent inhibitor of pannexins in mammalian cells; an effect completely unexpected in an antibiotic that is known to affect bacterial replication. Most importantly, the study 1 reported that trovafloxacin altered the fragmentation of cells in smaller pieces that occurs during apoptosis. This effect was tested at the drug concentrations in the blood that were used in treatment with patients.
Thus, the study established that pannexin channels control the timing of dying cells falling apart and that this process is specifically inhibited by the antibiotic trovafloxacin. Given how essential apoptosis is for life, one of the obvious questions raised by this study is whether this off-target action of the antibiotic could be responsible for the terrible side effects seen in patients. However, it is possible that this will never be known.
But there is another important implication of this work, which might hold the promise for an improved design of antimicrobial therapies. According to the WHO, antibiotic resistance is a major health issue responsible for the complication the treatment of tuberculosis or common infections (e.g. urinary tract infections, pneumonia, bloodstream infections). Since quinolones, the family to which trovafloxacin belongs, represent some of the most commonly prescribed antibiotics it is possible that the risk of side effects could be tackled by chemically altering the toxic parts so that they do not affect mammalian tissues, but preserving the antibacterial effect.
Only time will tell whether the surprising link found between a toxic antibiotic and the process of mammalian cell death helps improving antimicrobial therapies. The never-ending story of trovofloxacin stands as a clear example of how the unexpected is still possible in biology.
References
- Poon I.K.H., Allison J. Armstrong, Jason M. Kinchen, Ignacio J. Juncadella, Douglas A. Bayliss & Kodi S. Ravichandran (2014). Unexpected link between an antibiotic, pannexin channels and apoptosis, Nature, 507 (7492) 329-334. DOI: http://dx.doi.org/10.1038/nature13147 ↩
2 comments
[…] para asegurar el buen funcionamiento del conjunto del organismo en un fenómeno llamdo apoptosis. You have to learn how to die por Guzmán […]
[…] bermatzeko. Fenomeno honi apoptosia esaten zaio eta Guzmán Sánchezek hitz egin digu honetaz You have to learn how to die […]