Drug combinations to combat antibiotic resistance
One of the biggest health threats in our current society is not related to a virus, not even to diabetes or cardiovascular disease, but to antimicrobial resistance. In fact, over 5 million deaths per year are associated with resistant bacteria, of which nearly 1.3 million deaths per year are directly attributable to antimicrobial resistance. This requires the development of new approaches to combat antibiotic resistance.
A recent study 1 published in Nature Microbiology shows the results from a systematic analysis of the effects of over 10,000 drug combinations against common multidrug-resistant bacteria. Although using drug combinations is not rare in clinical practice, so far no one had performed such a wide screening of combinations of different classes of antibiotics, or combinations of antibiotics and non-antibiotic drugs.
Testing the direct effects of drug combinations on bacteria is important, because due to their different cellular targets, their effects could either complement (synergising) or antagonise each other. Although the latter may be seen like a negative effect, it could actually be beneficial to avoid the collateral damage caused by antibiotics to “good” gut bacteria.
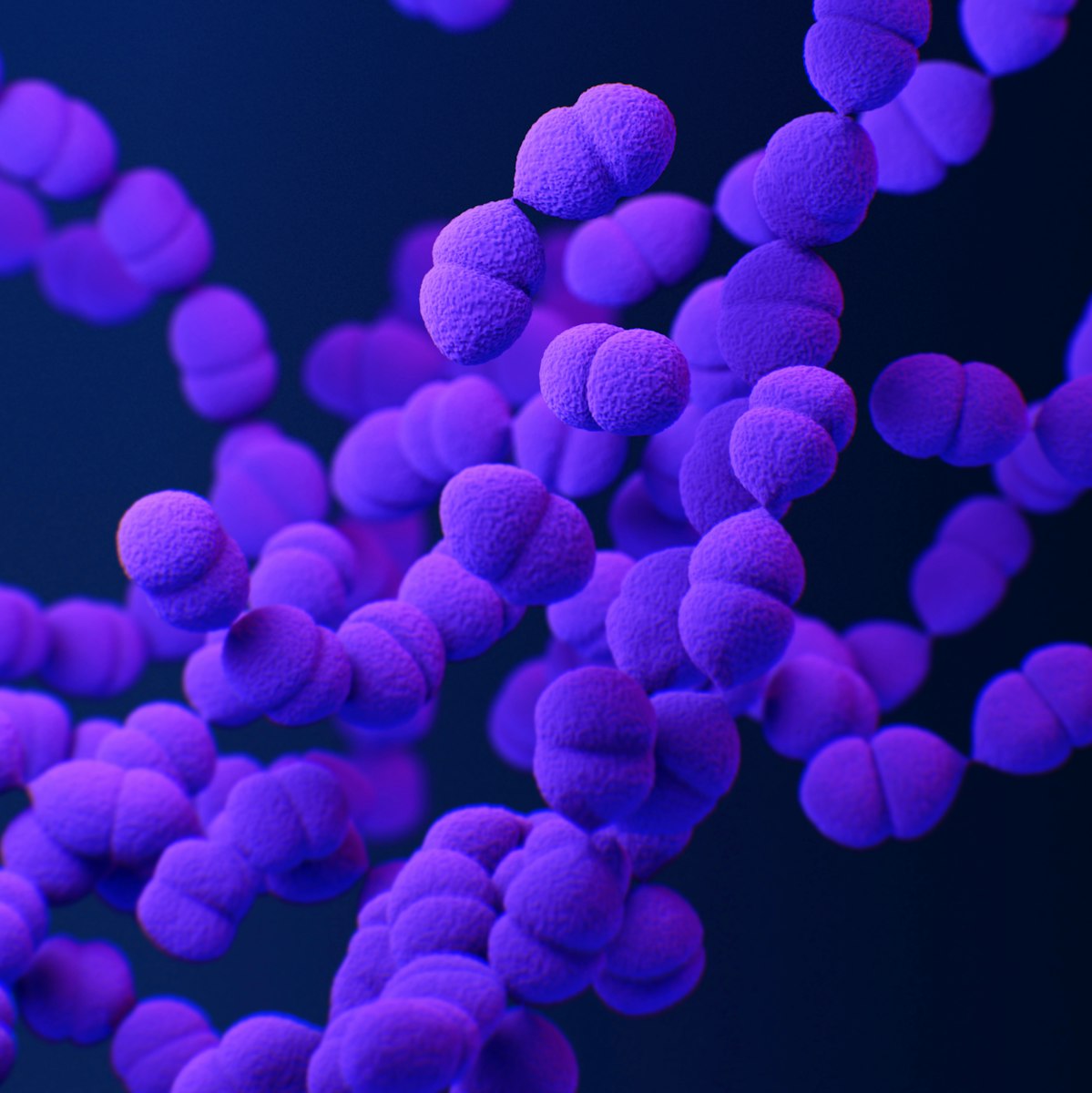
Although a similar study was previously performed in Gram-negative bacteria such as E. coli, this time the team focused on Gram-positive bacteria such as Staphylococcus aureus or Streptococcus pneumoniae, as these bacteria not only have a different cellular structure to Gram-negative but they are also responsible for severe, deadly infections.
To test over the over 8,000 combinations of 65 different antibiotics, spread across all major classes as well as the over 2,500 combinations of antibiotic drugs with non-antibiotic drugs in three different bacterial species, the researchers used a robotics setup to assist with the work and increase reliability. Using this approach, they could identify more than 1000 interactions, including both positive and negative. Not only were the effects highly species- and even strain-specific but also distinct from the interactions observed for Gram-negative bacteria. To test the validity of their in vitro assay in vivo, they infected moth larvae with the pathogens and evaluated the effects of specific drug combinations.
This dataset can revolutionise the treatment of bacterial infections and help combat antibiotic resistance, particularly because the researchers have made this data publicly available. In the future, using this kind of approaches might assist both clinical development and clinical practice and may help deal with the deleterious effects of antimicrobial resistance.
References
- Cacace, E., Kim, V., Varik, V. et al. (2023) Systematic analysis of drug combinations against Gram-positive bacteria. Nat Microbiol doi: 10.1038/s41564-023-01486-9 ↩