When the inhibition of the inhibitory signals results in an exacerbated response. The case of IL-13 and the COVID-19 severity.
Author: José R. Pineda got his Ph.D. from University of Barcelona in 2006. Since 2007 he has worked for Institut Curie and The French Alternative Energies and Atomic Energy Commission. Currently he is a researcher of the UPV/EHU. He investigates the role of stem cells in physiologic and pathologic conditions.
A long time ago, I started my PhD on Huntington’s disease, a fatal neurodegenerative disorder with no cure. A general reasoning at that time was that during the evolution of this neurodegenerative disease, a subtype of inhibitory neurons of the neural circuits began to die. The result was that the loss of the inhibitory neurons deregulated the neural circuits, as the excitatory neurons were not properly controlled. In turn, the lack of control of the excitation provoked neural excitotoxicity, entering thus into a vicious loop of the neural circuit for both neural populations. Now, almost 20 years after this initial reasoning, a parallelism can be extrapolated to intercellular communication when we think about the progression of severity of COVID-19.
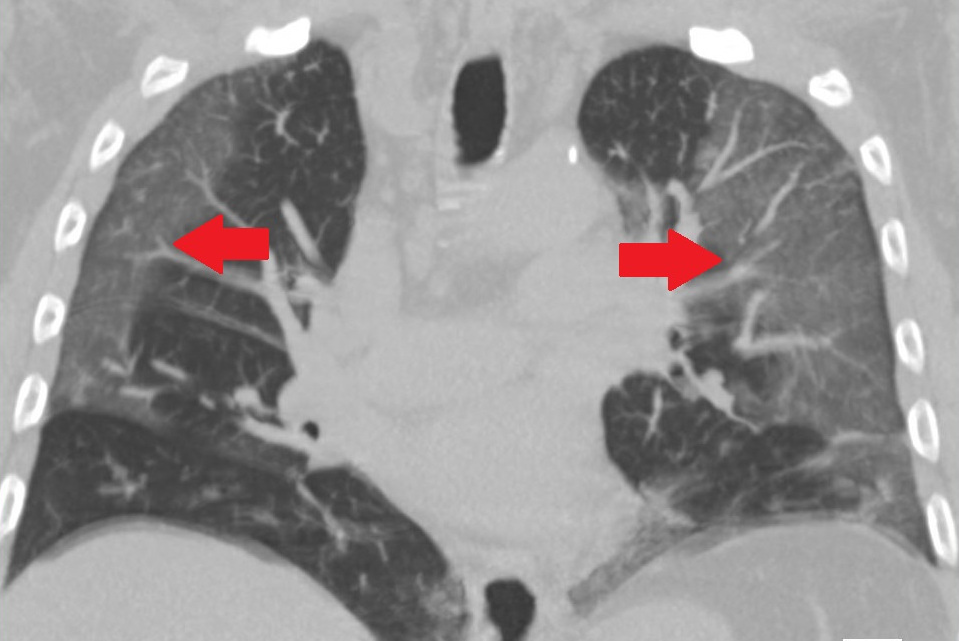
The human body is a machine of precision, where all the signals and cellular behavior is finely controlled. The dysregulation not properly controlled can cause a snowball that rapidly evolves into a chain-reaction driven events that could end with a collapse. Immune dysregulation is characteristic of the more severe stages of COVID-19. The work published by Alexandra N. Donlan in the Journal of Clinical Investigation deciphers one of the key events that pave the way to understand the mechanisms by which the cellular dysregulation contributes to the severity of COVID-19 1. Using a heatmap, they found an interrelation with elevated levels of a signal mediator called interleukin 13 (IL-13) and the need of mechanical ventilation in two independent patient cohorts. IL-13 draw their attention because this interleukin is implicated in the recruitment of white blood cells to the lungs, increase mucus secretion in the airway epithelia and fibrosis through collagen deposition, becoming responsible for pathogenic responses in the lungs. Moreover, other additional studies demonstrated that IL-13 increases from day 5 to 20 of illness in severe COVID-19 patients that require intensive care unit or mechanical ventilation 2. Other associated characteristic was the increase of hyaluronan (a polysaccharide that regulates cell adhesion, motility 3 4 and mediates cell proliferation and differentiation 5) in both lungs and plasma. When they reproduced the infection in a murine model, the analysis of RNAseq at 5 days post-infection of infected lungs showed an upregulation of transcripts from genes coding for IL-4 and IL-13. As they observed an association of IL-13 but not IL-4 with severe disease in patients, they decide to focus the study in IL-13 interleukin.
The first experiment that they carried out to check the role of IL-13 was to neutralize it by intraperitoneal injection of antibodies designed specifically to block IL-13 in infected mice. IL-13 neutralization reduced the disease severity, observing less weight loss and mortality independently of the viral load, although histological analysis did not change lung tissue damage. This result suggested that the amelioration of the disease was not due to reduced infectious particles, but likely due to the events triggered by IL-13 signalling. To further gain insight about the mechanistic after IL-13 neutralization they did again RNA-seq analysis of whole lung tissue but this time, comparing IL-13-neutralized samples from control samples. They found a strong reduction of gene expression hyaluronan synthase 1 in IL-13-neutralized condition meanwhile it was upregulated in non-treated infected mice. Furthermore, the enzyme hyaluronidase responsible to break down endocytosed hyaluronan were upregulated during the course of the infection. These findings support the pathological role of hyaluronan in humans with COVD-19. To confirm the role in the disease, they proceed with the intranasal administration of IL-13 in healthy mice provoking an increase of hyaluronan deposition in the lungs and increased levels in serum. These results indicated that hyaluronan production and signalling are downstream of IL-13 and supported the role of the interleukin in the regulation of the hyaluronan deposition and accumulation in the lungs. It is noteworthy to state that excessive levels of hyaluronan are able to bind large amounts of water and could contribute to impair oxygen uptake or result in edema, both affections characteristic of COVID-19 hospitalized severe patients.
One way to test if hyaluronan have an additional participation on physiopathological function on lungs is to block its receptor. The hyaluronan receptor is the “CD44” or “cluster of differentiation 44”. Donlan and collaborators blocked CD44 from days one to four post-infection, and they observed a reduced mortality in infected mice and an amelioration of clinical scores. Interestingly, patients with asthma also have elevated levels of CD44 6, the results of this work demonstrates the role of immune response, highlighting the importance of the role of IL-13, and the downstream hyaluronan accumulation in respiratory failure and warrants further research for immunotherapy of lung diseases. However, it’s necessary to keep in mind that given the heterogeneity of immune responses to COVID-19, IL-13 blockade may not work in all treated patients. However, given that this signalling pathway is also observed in allergic or asthmatic inflammation, future treatments will also help with these lung affections.
References
- Donlan AN, Sutherland TE, Marie C, Preissner S, Bradley BT, Carpenter RM, Sturek JM, Ma JZ, Moreau GB, Donowitz JR, Buck GA, Serrano MG, Burgess SL, Abhyankar MM, Mura C, Bourne PE, Preissner R, Young MK, Lyons GR, Loomba JJ, Ratcliffe SJ, Poulter MD, Mathers AJ, Day AJ, Mann BJ, Allen JE, Petri WA Jr. 2021. IL-13 is a driver of COVID-19 severity. JCI Insight. 150107. Online ahead of print. PMID: 34185704 DOI: 10.1172/jci.insight.150107 ↩
- Carolina Lucas, Patrick Wong, Jon Klein, Tiago B R Castro, Julio Silva, Maria Sundaram, Mallory K Ellingson, Tianyang Mao, Ji Eun Oh, Benjamin Israelow, Takehiro Takahashi, Maria Tokuyama, Peiwen Lu, Arvind Venkataraman, Annsea Park, Subhasis Mohanty, Haowei Wang, Anne L Wyllie, Chantal B F Vogels, Rebecca Earnest, Sarah Lapidus, Isabel M Ott, Adam J Moore, M Catherine Muenker, John B Fournier, Melissa Campbell, Camila D Odio, Arnau Casanovas-Massana, Yale IMPACT Team; Roy Herbst, Albert C Shaw, Ruslan Medzhitov, Wade L Schulz, Nathan D Grubaugh, Charles Dela Cruz, Shelli Farhadian, Albert I Ko, Saad B Omer, Akiko Iwasaki. 2020. Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature. Aug;584(7821):463-469. PMID: 32717743 DOI: 10.1038/s41586-020-2588-y ↩
- Dowthwaite GP, Edwards JCW, Pitsillides AA. 1998. An Essential Role for the Interaction Between Hyaluronan and Hyaluronan Binding Proteins During Joint Development. J Histochem Cytochem. 46(5):641-651. PMID: 9562572 DOI: 10.1177/002215549804600509 ↩
- Cheung W, Cruz TF, Turley EA. 1999. Receptor for hyaluronan-mediated motility (RHAMM), a hyaladherin that regulates cell responses to growth factors. Biochem Soc Trans. 1999 Feb;27(2):135-42. PMID: 10093722 DOI: 10.1042/bst0270135 ↩
- Entwistle J, Hall C, Turley E. 1996. Hyaluronan receptors: regulators of signalling to the cytoskeleton. J Cell Biochem.(61):569–77. PMID: 8806080 DOI: 10.1002/(sici)1097-4644(19960616)61:4<569::aid-jcb10>3.0.co;2-b ↩
- Marc E Rothenberg. 2003. CD44–a sticky target for asthma. J Clin Invest. May;111(10):1460-2. PMID: 12750395 DOI: 10.1172/JCI18392 ↩