Cognitive and brain changes due to SARS-CoV-2
Cognitive and brain changes due to SARS-CoV-2
Author: José R. Pineda got his Ph.D. from University of Barcelona in 2006. Since 2007 he has worked for Institut Curie and The French Alternative Energies and Atomic Energy Commission. Currently, he is a researcher of the UPV/EHU. He investigates the role of stem cells in physiologic and pathologic conditions.
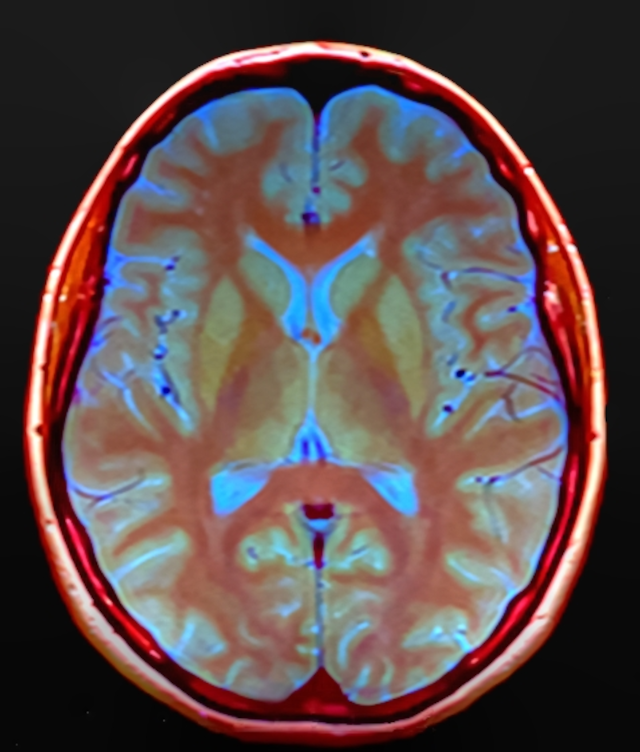
In a previous work Jenny Meinhardt and Frank L. Heppner showed that SARS-CoV-2 virus was able to use nasal mucosa as an entry towards central nervous system, revealing the fact that SARS-CoV-2 was able to reach the brain 1. Now, a recent study led by Gwenaëlle Douaud and collaborators published in Nature, describe for the first time, changes in brain structures even after mild infection 2. To reach this conclusion, they created a biobank of brain imaging data from 785 participants and then compared a group of control subjects towards a group of interest (401 individuals) in which they obtained two scans, one before the SARS-CoV-2 infection and the other 38 months after infection. Interestingly, Douaud and collaborators found a greater reduction in brain limbic regions. Limbic regions are parts of the brain involved in our behavioural and emotional responses. Particularly the differences were in grey matter thickness (the structural region where reside the body of the neurons), tissue-contrast in the orbitofrontal cortex (a region involved in the cognitive process of decision-making) and para-hippocampal gyrus (region responsible for memory encoding and retrieval). Furthermore, the greatest changes were observed in markers of tissue damage in regions functionally-connected to the primary olfactory cortex, converging into a significant reduction in global brain size.
Taken into account the role of the mainly affected brain regions, they correlated that the observed structural alterations could be compatible with the phenotypic and cognitive decline reported of the individuals. To quantify these alterations, they used the top most significant tests to detect differences between out-of-sample (pre)dementia cases and healthy controls. These tests are the Trail Making Test (test used to assess attention, flexibility of thought and visuospatial ability). It consists of two parts: in the first you have to quickly join the numbers with lines, these being randomly placed in numerical order and in the second you have to join the numbers and letters with lines, these being randomly placed, for example joining 1 with the A, the 2 with the B, etc. 3. The Symbol Digit Test (test used to assess psychomotor speed, which measures processing speed as well as motor speed). It is a paper-pencil measure, which requires an individual to substitute digits for abstract symbols using a reference key 4. The fluid intelligence score (fluid intelligence involves reasoning and problem-solving for problems to which familiar solutions are not available), generally the fluid-intelligence score decreases with age 5. The other two tests are the measure of reaction time (participants complete a timed test of symbol matching) and the measure of numeric memory (participants see a two-digit number which they were asked to recall after a brief pause. This increased by one until the participant made an error, or they reached the maximum of twelve digits), and the Pairs Matching test (a test used to detect discrimination where participants are asked to memorize the positions of six card pairs, and then match them from memory while making as few errors as possible. This test involves a learning paradigm for the assessment of hippocampal-dependent learning and memory processes) 6. To exclude the possibility of transitory changes due to a (general) viral infection, the authors also analyzed the effects of (non-related to COVID-19) pneumonia and influenza virus.
From all the above-mentioned tests, the authors found a significantly greater increase of the time taken to complete Trails A (numeric) and B (alphanumeric) of the Trail Making Test in the SARS-CoV-2 infected group. Indeed, considering the age-modulation of the patients, the time to complete Pairs Matching round, showed a trend difference at baseline. Although this investigation showed some significant group differences in brain imaging-derived phenotypes (IDPs), no overlap of those IDPs were found for SARS-CoV-2 excluding the possibility to have a significant impact. Now, it should be very interesting to track the evolution during the lifetime in order to check if infected individuals could suffer greater cognitive deterioration during ageing. In the worst scenario, the overlapping olfactory- and memory-related functions of the regions shown to alter significantly over time in SARS-CoV-2 (hippocampi and perirhinal & entorhinal cortex) uncovers the possibility to be explored if long-term consequences of SARS-CoV-2 infection might in time contribute to any forms of dementia or even Alzheimer’s disease. On the opposite, it is noteworthy to mention that in previous waves of SARS-CoV-2 infection early neurological signs in COVID-19 such as hyposmia or hypogeusia (a reduced ability to smell or taste things) preceded the onset of respiratory symptoms in the majority of affected patients. These repeated sensory deprivation and anterograde degeneration from olfactory neurons is known to be sufficient to lead to loss of grey matter in olfactory-related brain regions. Maybe the pattern of longitudinal abnormalities observed in the limbic, olfactory brain regions of SARS-CoV-2 positive participants, if they are indeed related to olfactory dysfunction, might be attenuated over time if the infected participants go on to recover their sense of smell and taste. Be that as it may, we will need the passing of the years to finish understanding the real implications and long-term effects of this disease.
In conclusion, the use of the biobank data and the non-invasive automated analysis of longitudinal imaging study comparing brain scans acquired from individuals before and after SARS-CoV-2 infection, allowed to the researchers to have a considerable amount of cases able to define and detect subtle different sites of damage. These data could help to uncover possible spreading pathways associated with the infection and tracing of the effects of the disease within the brain during ageing of infected patients.
References
- Jenny Meinhardt, Josefine Radke, Carsten Dittmayer, Jonas Franz, Carolina Thomas, Ronja Mothes, Michael Laue, Julia Schneider, Sebastian Brünink, Selina Greuel, Malte Lehmann, Olga Hassan, Tom Aschman, Elisa Schumann, Robert Lorenz Chua, Christian Conrad, Roland Eils, Werner Stenzel, Marc Windgassen, Larissa Rößler, Hans-Hilmar Goebel, Hans R Gelderblom, Hubert Martin, Andreas Nitsche, Walter J Schulz-Schaeffer, Samy Hakroush, Martin S Winkler, Björn Tampe, Franziska Scheibe, Péter Körtvélyessy, Dirk Reinhold, Britta Siegmund, Anja A Kühl, Sefer Elezkurtaj, David Horst, Lars Oesterhelweg, Michael Tsokos, Barbara Ingold-Heppner, Christine Stadelmann, Christian Drosten, Victor Max Corman, Helena Radbruch, Frank L Heppner. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nature Neuroscience. 2020 Nov 30. doi: 10.1038/s41593-020-00758-5. ↩
- Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, Lange F, Andersson JLR, Griffanti L, Duff E, Jbabdi S, Taschler B, Keating P, Winkler AM, Collins R, Matthews PM, Allen N, Miller KL, Nichols TE, Smith SM. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022 Mar 7. doi: 10.1038/s41586-022-04569-5. ↩
- Reitan RM. The relation of the trail making test to organic brain damage. J Consult Psychol. 1955 Oct;19(5):393-4. doi: 10.1037/h0044509. ↩
- Beck at, Feshback S, Legg D. The clinical utility of the digit symbol test. J Consult Psychol. 1962 Jun;26:263-8. doi: 10.1037/h0049298. ↩
- Mohammed K Shakeel, Vina M Goghari. Measuring Fluid Intelligence in Healthy Older Adults. J Aging Res. 2017;2017:8514582. doi: 10.1155/2017/8514582 ↩
- Sarah Buck, Filipa Bastos, Torsten Baldeweg, Faraneh Vargha-Khadem. The Pair Test: A computerised measure of learning and memory. Behav Res Methods. 2021 Apr;53(2):928-942. doi: 10.3758/s13428-020-01470-9. ↩