Studying language in people with dementia
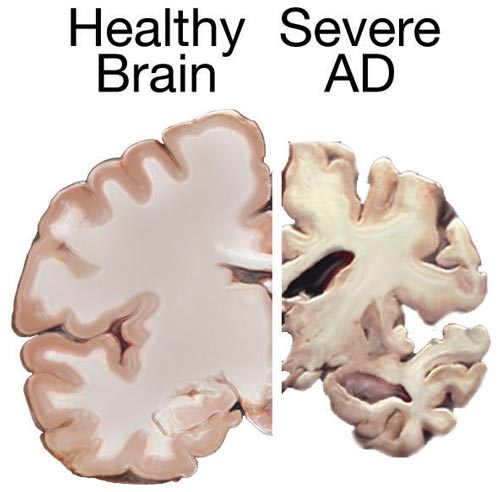
People who are diagnosed with dementia may initially report problems on memory and/or language that affect their activities of daily living. Once factors such as depression, delirium, or mild cognitive impairment, are disregarded, these people are typically referred to a neurologist, radiologist, and neuropsychologist or speech therapist who will help them to understand the reason for their complaints and who will refer them to treatment 1. These problems may become more severe over time, due to a deterioration of nerves cells in specific brain areas – see figure 1.
A percentage of these patients may present particular problems to produce written and spoken language as well as to comprehend it. These patients may be indicated to have frontotemporal dementia and later on, when language difficulties are particularly salient, they may be labelled as having primary progressive aphasia and categorized within three different main types: non-fluent/agrammatic, semantic, and logopenic 2.
The name of primary progressive aphasia was initially indicated by Marcel Mesulam in the 80s, now a professor of Neurology at Northwestern University, in the USA 3. Mesulam stems from a tradition where people with dementia had been described by Arnold Pick in 1982 and Alois Alzheimer in 1911 – surnames that may well remind the reader of progressive neurological diseases such as Pick’s disease and Alzheimer’s disease. Be it as it is, and with some more modern categorizations [3], the work of these researchers is still on vogue and will be more so within the next years, as the World Health Organization estimated “dementia rates will double every 20 years, reaching 115.4 million in 2015”4.
Considering this, and despite the fact of the rather notorious increase in population with dementia over the next years, there are certain aspects of dementia that are currently under consideration. Bang et al. [4], for example, indicated that the routine assessments that these patients undergo may not be sufficiently sensitive to predict the onset of the disease. Also, the classification of the different types of primary progressive aphasia may need of the work in collaboration of different researchers including behavioural scientists, neuroanatomists, neuropathologists, and geneticists. Furthermore, treatment of dementia with adjuvant measures, such as that of specific drugs or the use of non-invasive stimulation (e.g., transcranial direct electrical stimulation, transcranial magnetic stimulation), has a relatively short tradition, which makes these types of studies very appealing for researchers but yet not completely adaptable to the needs of specific patients or the coverage of health systems and private insurers.
In terms of language, each the three variants of primary progressive aphasia (i.e., non-fluent, semantic, logopenic) present different inclusion criteria which are worth reviewing, as they were only agreed upon until recently [2]. Furthermore, people which each of the three variants may be more prone to present damage in specific brain areas, which in a way may explain their behaviour and aid its therapeutical approach [4].
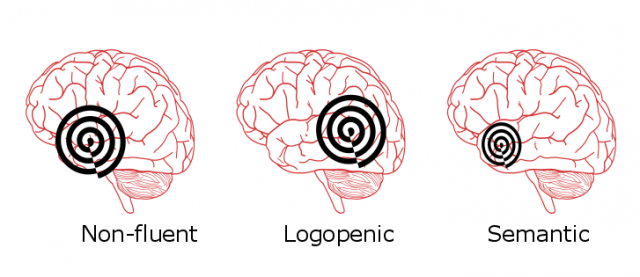
People with the non-fluent/agrammatic variant of primary progressive aphasia, are labelled as so, because they present effortful language production, characterized by problems in speech rate, due to deficits in producing words and building correct sentences. Some of these patients may also present difficulties in articulating the correct phonemes in words (what is called, apraxia of speech). There are other features that characterize these patients, mostly, difficulties in sentence comprehension, and absence of errors in single-word comprehension and object knowledge such as understanding what do we refer when we talk about a “table” and what are the physical and usage features of the object (e.g., it can be made of wood, we use it to sit and work/eat, etc.). These patients typically present further damage in the anterior part of the temporal lobe and the insula.
People with the semantic variant of primary progressive aphasia may present particular problems at naming words when seeing a picture or being presented with some other stimulus (e.g., a sound, a smell, etc.). Also, they may have particular difficulties in comprehending single words – which is in contrast with the non-fluent/agrammatic variant, which does not present problems in this latter task. Some of these patients may also present problems with reading and writing and present no problems in word repetition, or general speech production (be it to produce correctly formed sentences, as well as to articulate them). These patients typically present further damage in the posterior part of the temporal lobe and the inferior part of the parietal lobe.
Finally, people with the logopenic variant of primary progressive aphasia may present problems in producing single words in naming tasks, as well as in everyday conversations. Also, they have difficulties repeating sentences. Some of these patients may have deficits in comprehending single words and understanding objects (similarly to the semantic variant), have no problems in articulating words (as opposed to the semantic and the non-fluent variants), and neither present difficulties in producing language in everyday contexts. These patients present further damage in the anterior part of the temporal lobe and, in advanced stages, in the inferior part of the frontal lobe (the so called, orbitofrontal cortex).
With this information in mind, language researchers are currently working to improve the current routine assessments, for example, by coming up with protocols that include many different language tasks, hence, allowing the assessment of very diverse language capacities (e.g., phonology, semantics, lexical retrieval, morpho-syntax, etc.). Other researchers are also working on dedicated tasks to assess this population, and on the use of neuroimaging methods such as electroencephalography and functional magnetic resonance imaging, to obtain other and sometimes more objective information over the performance of patients. Another aspect that is currently put to play is differences between specific word categories over different brain areas be it in naming tasks or in everyday conversations. This is the case, for example, of nouns/objects such as “table” which may have a stronger representation in the temporal lobe, and verbs/actions which may be better processed in the frontal and parietal lobe.
As a whole, studying language in people with dementia is a very exciting field of research, which will bring a lot of knowledge over how the brain works while making sure we gain the means to assess and treat people with this progressive disease. This work could not exist without a collaborative blend of (clinical) linguists with many other clinical and research figures.
References
- Cummings, J. L. (2008). The Black Book of Alzheimer’s Disease, Part 2.Primary Psychiatry, 15(3), 69. ↩
- Gorno-Tempini, M. L., Hillis, A. E., Weintraub, S., Kertesz, A., Mendez, M., Cappa, S. E. E. A., … & Grossman, M. (2011). Classification of primary progressive aphasia and its variants. Neurology, 76(11), 1006-1014. ↩
- Mesulam, M. (2001). Primary progressive aphasia. Annals of neurology, 49(4), 425-432. ↩
- Bang, J., Spina, S., & Miller, B. L. (2015). Frontotemporal dementia. The Lancet, 386(10004), 1672-1682. DOI: 10.1016/S0140-6736(15)00461-4 ↩