Psychosis and brain structure
One of the intriguing and central mysteries in contemporary neuroscience revolves around the intricate relationship between the brain and the mind. While our understanding of neurons, neurotransmitters, and neuronal receptors has advanced significantly, the elusive question remains: How do these complex chemical and electrical processes translate into thoughts, emotions, and behaviors? Gaining insight into these processes is crucial not only for unravelling the mysteries of the mind, but also for comprehending the intricacies of a diseased brain.A compelling example lies in the realm of psychosis, a broad term encompassing mental states characterized by a detachment or loss of contact with reality.
In such instances, an organism receives sensory data from its environment, and the brain, ostensibly armed with accurate information, constructs an erroneous interpretation. The quandary arises when we confront a mind seemingly malfunctioning. The pivotal question emerges: Can we discover a neurological signature of mental illness within the brain?
Consider the case of “Mr. House,” a 22-year-old man without a psychiatric history, seeking help at the emergency department accompanied by his family 1. He is in his final year at university. According to his sister, the patient has been harboring delusional beliefs, perceiving himself as a superhero, and alleging that his college roommates are discussing it. Additionally, he experiences paranoid thoughts, suspecting that his university room is under surveillance. During his interaction with the psychiatrist, he reveals plans to meet with the President of the United States the following day. The patient also exhibits periods of incoherent speech.
The patient underwent a comprehensive examination, including a urine analysis to detect the presence of drugs. No significant findings emerged, and the physical examination revealed no focal neurological abnormalities. The diagnosis pointed to a first episode of psychosis.
It’s essential to clarify that a psychotic episode is not an extraordinary occurrence. Many individuals undergo unusual experiences or exhibit distortions of reality at some point in their lives without hindering their ability to lead normal lives or causing distress. The severity varies, with some experiencing particularly intense episodes, but these are not markedly different from the experiences of others.
Psychosis symptoms encompass not only reality distortion but also disorganization, cognitive function deterioration, abnormal psychomotor behavior, delusional thoughts, and thought disorders affecting language’s semantic and syntactic relationships. Psychosis may manifest in conditions such as schizophrenia, schizoaffective disorder, depression, bipolar disorder, Alzheimer’s, Parkinson’s, multiple sclerosis, epilepsy, and even non-celiac gluten sensitivity.
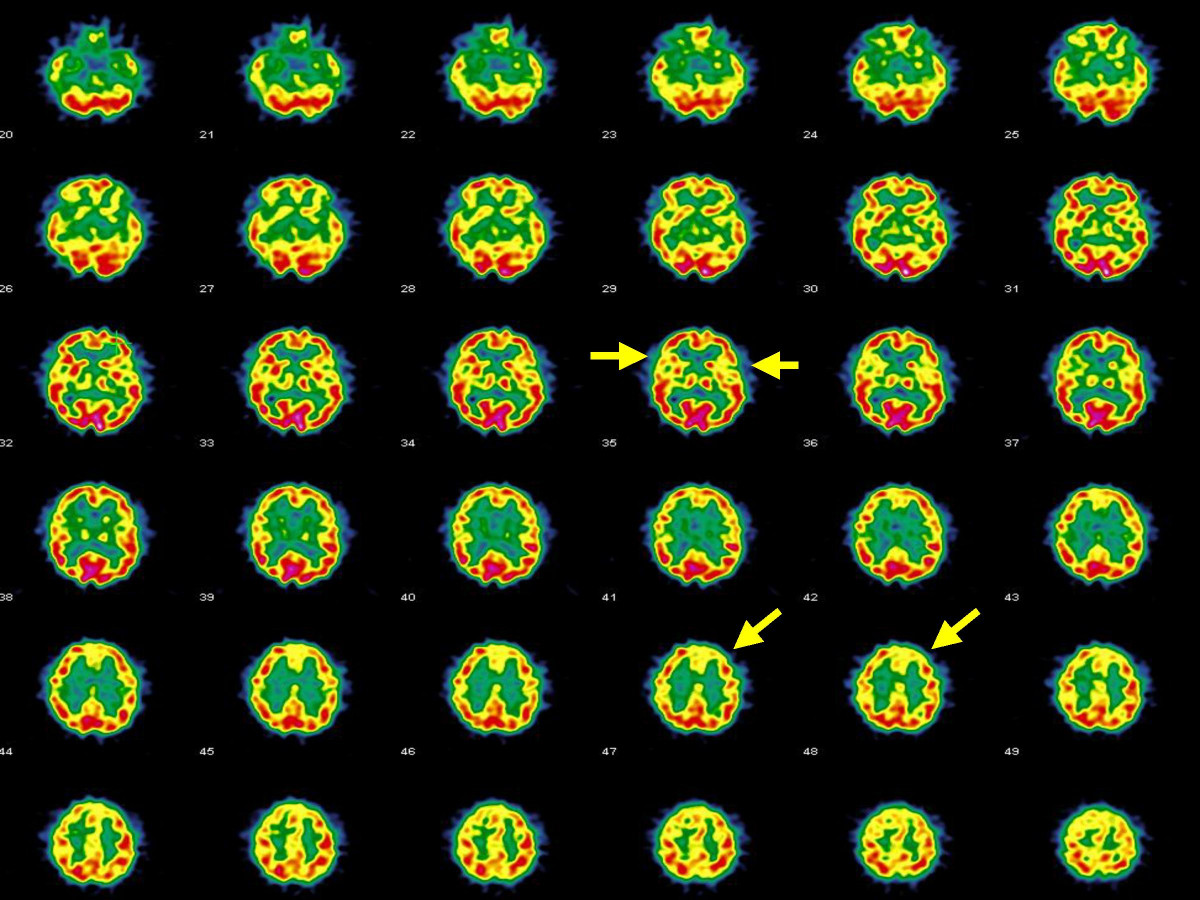
Concerned about Mr. House’s condition, his family inquired about the necessity of a neuroimaging brain study. Modern techniques permit non-invasive observation of the brain’s functioning without causing harm. However, the question remains: Is it valuable? Does a psychotic brain exhibit observable changes? Currently, there is no consensus on whether an MRI study provides informative insights during a first episode of psychosis. While some clinical guidelines advocate for examining all patients, others suggest doing so only when a secondary cause of psychosis is suspected. Not all individuals with psychosis display neurological alterations, and some otherwise healthy individuals may present anomalies such as white matter hyperintensity, associated with cognitive impairment and elevated cerebrovascular and mortality risks.
To address this uncertainty, Blackman and colleagues conducted a meta-analysis to investigate the frequency and presence of intracranial abnormalities in first-episode psychosis (FEP) patients 2. They categorized radiological abnormalities based on clinical relevance, considering changes that would impact treatment or diagnosis. Subgroups included white matter, vascular, ventricular, cystic, pituitary, tumor, and cerebral atrophy anomalies.
After scrutinizing 240 publications, around 12 studies (13 samples) met inclusion criteria, involving 1618 FEP patients. Clinically relevant abnormalities were reported in 9 studies (1318 patients), and 8 studies included healthy controls (1866 total controls).
The pooled prevalence of any abnormality was 26%, with heterogeneity between studies being high. Clinically relevant abnormalities had a prevalence of 5.9%, with moderate heterogeneity. White matter (7.9%) and ventricular anomalies (typically enlargement, 5.0%) were the most prevalent. Clinically relevant abnormalities were primarily in white matter (0.9%) and cysts (0.5%).
Compared to healthy controls, FEP patients were nearly three times more likely to exhibit any radiological abnormality and 1.5 times more likely to display a clinically relevant abnormality. The study concluded that 18 patients needed screening to detect one clinically relevant abnormality.
The study’s strengths include exploring potential moderating factors and comparing abnormalities between FEP and controls. Limitations include the inclusion of MRI studies as part of the investigation and the exclusion of patients with evidence of a possible secondary cause of psychosis. Longitudinal follow-up data were unavailable.
Given the increased accessibility and decreased cost of MRI, the study supports the feasibility of offering neuroimaging studies to patients experiencing a first episode of psychosis.
References
- Miller B (2023) Prevalence of Neuroradiological Abnormalities in First-Episode Psychosis. Psychiatric Times ↩
- Blackman G, Neri G, Al-Doori O, Teixeira-Dias M, Mazumder A, Pollak TA, Hird EJ, Koutsouleris N, Bell V, Kempton MJ, McGuire P (2023) Prevalence of neuroradiological abnormalities in first-episode psychosis: a systematic review and meta-analysis JAMA Psychiatry ↩