Watch your language! Linguistic factors contributing to COVID-19 spread
Watch your language! Linguistic factors contributing to COVID-19 spread
Authors: Natalie Grant & Lena Burkel, students of the European Master’s in Clinical Linguistics & Adrià Rofes, assistant professor of neurolinguistics at the University of Groningen
By now, we’re all experts in the common symptoms of the oh so omnipresent COVID-19 – say, for example, dry coughing, fever, and loss of smell (Sauer, 2021). While we’re all hyper-vigilant about these symptoms, a new factor behind the spread of this virus may be on the rise: language. That’s right: new research suggests that the way we speak may modulate the spread of COVID-19 (Georgiou et al., 2021).
As we know, COVID-19 is a respiratory disease and its transmission depends on tiny droplets or liquid particles that are produced during any respiratory activity, such as breathing, coughing, or talking. These droplets may then be inhaled by a person standing close by, and the cycle continues.
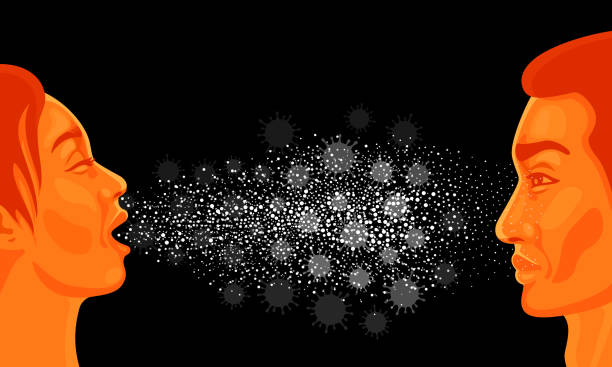
A study from Asadi et al. (2020) found that even just breathing and speaking can affect the number of droplets emitted. But that’s not all: they found that even more particles can be emitted when speaking and breathing over time in comparison to coughing and sneezing – just another good reason to always put on that mask! With speech and communication being fundamental parts of the human condition, it’s no wonder that researchers are interested in its role in respiratory disease transmission.
Considering that we possibly emit infectious droplets by the utterances we make, a study published back in 2003 in the Lancet already drew connections between the SARS virus (COVID – 19’s deadlier, but less contagious older sister) and aspiration among English and Japanese speakers.
Adding to this research, Asadi et al. (2020) also stressed the importance of speech sound characteristics in different languages in regards to respiratory disease transmission:
Aspiration can be observed in sounds such as /p/ where the air flow is shortly stopped before uttering the sound. We can imagine it like a “puff” of air. These puffs release more droplets and have therefore been assumed to contribute to the increased spread of respiratory diseases. Since the publication of the aforementioned Lancet article, however, the role of aspiration in respiratory disease transmission has been mixed.Iin fact, current studies on COVID-19 show that aspiration isn’t that significant of a factor after all (Georgiou et al., 2021).
Another aspect is voicedness – voiced speech sounds include vowels and nasals plus a few consonants like /b/, /g/ and /d/. Asadi et al. (2020) looked at voicedness and found that the vowel /i/ (like for example in “need” or “sea”) produced more particles in comparison to vowels like /a/ and /u/. Indeed, all vowels seem to be better conduits for transmission when compared to consonants, because of their voiced quality.
These same researchers also found a correlation between the vowel/consonant ratio of a language and particle emission. We can take an example from a European language: Italian has a comparatively high vowel density (48%) when compared to English, German, Spanish and French, meaning almost every second letter is a vowel (Duden 2020). In fact, the most common vowel in Italian is /i/. This factor alone, however, is certainly not the only reason why Italy has been one of the hardest hit European countries. A significantly long-life expectancy (meaning lots of old people), an overly dense population, and a smaller perception of personal space, could have all contributed to the swift spread of COVID-19 in the country (Bellegoni, 2020).
What does seem to make a difference, though, is amplitude. Amplitude can be thought of as the loudness of our speech. And research shows: the louder the voice, the higher the number of droplets (Asadi et al., 2020). One example that made headlines was covered in a study from Hamner et al. (2020), who reported on an account from Washington state where one individual infected with COVID-19 infected 52 others at a 2 ½ hour choir rehearsal. Two people died. As a result, many countries followed suit by prohibiting events requiring “loud” talking or singing such as church services, concerts, and theater. A question that follows is whether individuals who speak louder, or languages that are commonly spoken in a louder manner may have higher infection rates.
Despite these interesting linguistic arguments, as of today, there just isn’t enough evidence to pinpoint that certain languages are better at transmitting the virus than others. Needless to say, there are many non-linguistic factors in the mix (e.g., the source of transmission, such as touching infected surfaces and then the eyes or nose, (Georgiou et al., 2021) or average distance between speakers, (Asadi et al., 2020)). Now, when it comes to language one thing seems evident: it’s not what you say, but how you say it.

References
Asadi, S., Wexler, A. S., Cappa, C. D., Barreda, S., Bouvier, N. M., & Ristenpart, W. D. (2020). Effect of voicing and articulation manner on aerosol particle emission during human speech. PLOS ONE, 15(1), e0227699. doi: 10.1371/journal.pone.0227699
Belligoni, S. (2020, March 26). 5 reasons the coronavirus hit Italy so hard. The Conversation.
Duden. (2020). Kleines Kuriositätenkabinett der deutschen Sprache [Eng.: Small cabinet of curiosities of the German Language]. Bibliographisches Institut GmbH.
Georgiou, G. P., Georgiou, C., & Kilani, A (2021). How the language we speak determines the transmission of COVID-19. Irish Journal of Medical Science (1971-), 1-6. doi: 10.1007/s11845-020-02500-3
Hamner, L., Dubbel, P., Capron, I., Ross, A., Jordan, A., Lee, J., Lynn, J., Ball, A., Narwal, S., Russell, S., Patrick, D., & Leibrand, H. (2020). High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice — Skagit County, Washington, March 2020. MMWR. Morbidity and Mortality Weekly Report, 69(19), 606–610. doi: 10.15585/mmwr.mm6919e6
Inouye, S. (2003). SARS transmission: language and droplet production. The Lancet, 362(9378), 170. doi: 10.1016/s0140-6736(03)13874-3
Sauer, L. M. (2021, April 06). What Is Coronavirus? Johns Hopkins Medicine.