Mapping placebo: learning to self-care

Another busy day unfolds through dozens of medical visits, prescriptions, and auscultations. The next patient, a medication-resistant chronic back pain case, enters the office and asks the doctor whether acupuncture has something to do with placebos. The physician feels like the artful and evidence-based bedrocks of his medical praxis are called into a tug-of-war. A quote he has just read in a sugar packet envelope, allegedly said by Sigmund Freud, reverberates in his mind. “Modern science has not yet produced a calming medicine as effective as some kind words”. The doctor wonders to what extent calming words would help his patient dealing with pain.
We saw in the previous article what the placebo effect is and the somewhat conflicting views among biomedical scientists on its regard. Now, it is time to know in what manner we know it is a real entity and its possible clinical scope.
The starting point is a well-known fact in clinical drug development research: patients receiving placebos usually improve. The obvious conclusion, that patients through the interaction with physicians can cure themselves without the need of medicament, is however not broadly hold by scientists, despite the debate.
In general, the available research shows that placebos do not target the root of diseases, but rather their manifestations. The crucial point might seem a simple nuance, but its consequences are huge. “Cure is different from care”, explains Fabrizio Benedetti, a neuroscientist at the University of Turin who has been investigating placebo for more than 20 years. “I do not think a placebo can stop the neurodegenerative process in Parkinson´s disease. What we are talking about here is symptoms”, the researcher adds.
A study led by Benedetti in 2001 showed that placebos could help patients coping better with symptoms – even if symptoms stay untouched. The study aimed to assess a possible pain relief effect of a placebo intervention (a saline injection). At least two groups of patients were compared, one was told the saline injection was a potent painkiller while the other group received no information 1.
The placebo intervention did not change the pain intensity experienced and reported by patients, who all had undergone thoracic surgery for lung cancer immediately before the saline injection (also, all of them had earlier received a minimal baseline analgesia). However, patients could ask at will further (real) analgesia when needed. And, intriguingly, those in the placebo group requested and consumed a 20% lesser amount during a three-day long postoperative period.
Why patients requested lesser analgesia if they had a same level of pain? Some researchers think that response bias is behind this paradox. Subjects involved in clinical research can attach and commit to trial results, or may be tempted to report an improvement that is expected to occur even if absent 2. This issue is only sorted out in blinded studies in which both patients and observers who assess outcome ignore the actual treatment in each individual. But placebo studies can be at most only half blinded since patients must know what they are receiving. Actually, when patients ignore the treatment – this is another intriguing finding in placebo research – placebos and some active drugs substantially lose their effects.
In many placebo studies, it is, therefore, hard to know if we are in front of a genuine placebo effect or a response bias. However, does the issue necessarily mean the phenomenon is clinically irrelevant?
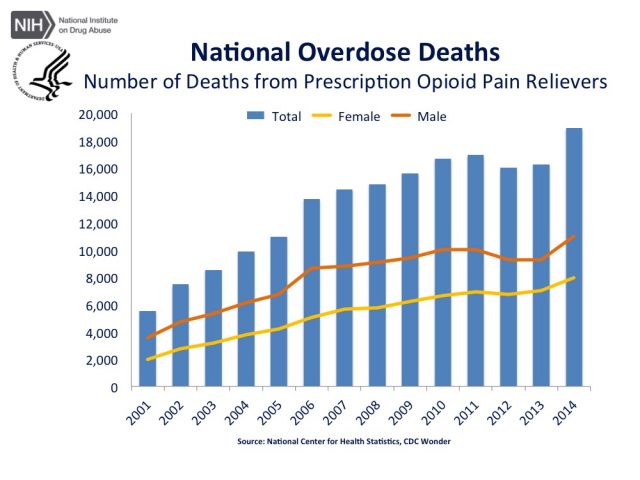
We saw earlier how placebos, over a no-intervention, led to a lower consumption of analgesia – a clinically meaningful finding given these drugs have several secondary effects (many of them are opioids that provoke addiction and other issues).
Setting aside the conundrum, how frequent the effect is? Does it apply to clinical conditions beyond pain? In 2010, a systematic analysis of placebo effects reviewed 202 earlier studies that had compared placebo versus non-intervention in 60 different clinical conditions 3. Overtly, considering more than 6000 patients analysed, placebos did not have huge health effects. However, the study showed a quite heterogeneous landscape when considering specific diseases, symptoms, and individuals.
Certain isolated conditions, pain, and nausea in particular, seemed susceptible of significant improvement by placebos. The effect, when present, was larger on outcomes reported by patients as compared to objective measures made by external observers, suggesting again that placebos influence symptoms rather than disease causes. Interestingly, most studies agreed to point a huge variability among individuals. Some subjects showed no response at all while the effect was large in others.
There would still be a chance for non-susceptible individuals if placebo responses could be learnt, a hypothesis explored in the last research led by Benedetti. In the study, published in February in The Journal of Physiology, researchers achieved to have a placebo imitating the effects of an anti-Parkinson agent on motor symptoms 4.
Surprisingly enough, a placebo managed to alleviate motor symptoms in Parkinson´s disease patients (assessed by neurologists blinded to the experimental condition) reaching the same effect size as an active substance called apomorphine (used against difficulties in movement and talk).
By itself, however, a first placebo administration was completely useless. The effect only happened when, before the placebo, patients had been exposed to the active agent. So patients could learn to show a placebo response, a finding, in turn, harder to interpret as a mere response bias.
So placebos could not replace active treatments (at least, in Parkinson´s disease), but might help fix some problems that limit their efficacy. Tolerance is a common issue (between 2-6% of opioid drugs used for chronic pain show this drawback) that reduces treatments´ therapeutic effects and arises when medications are used for a long period.
A joint regime of active drugs and placebos might thus help reduce consumption of drugs and tolerance issues if long-lasting learning of placebo responses would be viable – and still in last Benedetti´s research, the ability of placebo to mimic apomorphine lasted for no more than 24 hours. “This is surely a challenge for future research”, says Benedetti. “We still do not know how long the effect can last”, he adds. In his earlier studies in pain, however, conditioning could produce placebo responses for several days and up to 1 week.
Research still needs to establish in which contexts (if) and clinical conditions placebos could be helpful and to what extent. For granted, we cannot afford the risk of using ineffective treatments in conditions that can be lethal, but neither should we disregard any potential source of therapeutic effects for cases in which better alternatives are not available.
And there is still an unresolved concern that questions whether placebo interventions, if patient deception is involved, are even ethical. Is deception at all necessary in placebo interventions or does it really matter? Philosophers will help us navigate these issues in a next article.
References
- Pollo, A. et al (2001): Response expectancies in placebo analgesia and their clinical relevance. Pain, (93): 77-84. doi: 10.1016/S0304-3959(01)00296-2 ↩
- Hróbjartsson, A. et al (2011): Placebo effect studies are susceptible to response bias and to other types of biases. J Clin Epidemiol, 64(11): 1223–1229. doi:10.1016/j.jclinepi.2011.01.008. ↩
- Hróbjartsson, A. and Gøtzsche P.C. (2010): Placebo interventions for all clinical conditions. Cochrane Database Syst Rev. Jan 20;(1):CD003974. doi: 10.1002/14651858.CD003974.pub3 ↩
- Benedetti, F. et al (2016): Teaching neurons to respond to placebos. J Physiol, 1–14. doi:10.1113/JP271322 ↩
1 comment
[…] de los activos y de la salud comunitaria. Una vuelta de tuerca más sobre el placebo. En el blog Mapping Ignorance revisan algunos aspectos importantes sobre este tema, desde los problemas éticos hasta la […]