The origin of multiple sclerosis
In 1868, the famous, powerful and short French neurologist Jean-Martin Charcot, known as “the Napoleon of the Salpêtrière hospital”, described a new disease. He called it “sclerose en plaque” in reference to the numerous scars or sclerosis seen in the white matter of the brain and spinal cord. We now call it multiple sclerosis.
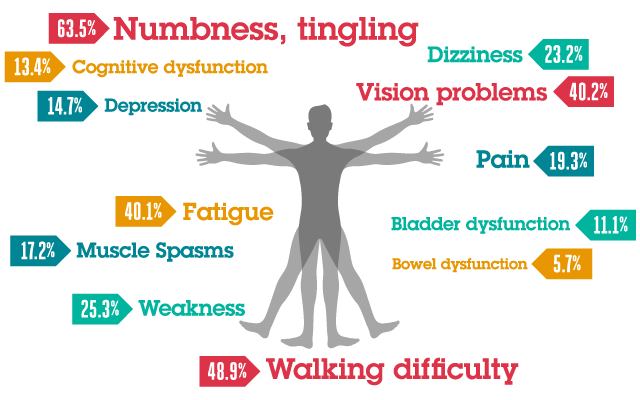
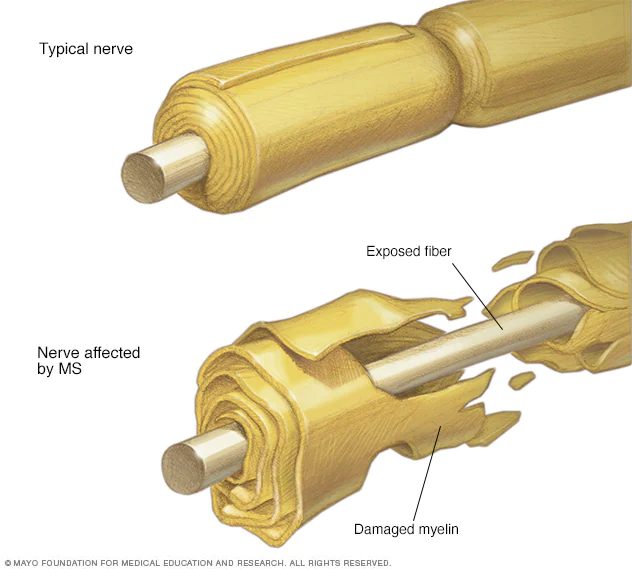
Multiple sclerosis is the most common demyelinating disease. Myelin is a fatty substance that surrounds the axons of many neurons, like the plastic that coats and insulates our electrical wires. In sclerosis, the myelin sheaths are damaged and these lesions alter the ability of parts of the nervous system to transmit signals, leading to a range of signs and symptoms, including physical, mental and sometimes psychiatric problems. Specific symptoms may include double vision, blindness in one eye, muscle weakness and problems with sensation or coordination. Thinking difficulties and emotional problems such as depression or mood instability are also common.
One of the great enigmas of multiple sclerosis was its origin. It is not considered a hereditary disease but there is a certain genetic propensity to suffer from this disease. There are risk factors such as smoking, and some other suspected ones such as stress, association with occupational exposures and toxins – mainly organic solvents, diet and hormone intake, but the evidence for their relationship to the disease is scanty and unconvincing. On the other hand, it has a very curious geographic pattern. Multiple sclerosis is more common in people living farther from the equator, although there are exceptions.
A new study has raised what may be the solution to the riddle of the origin of multiple sclerosis and the door to its solution. A study published in the journal Science by researchers at Harvard Medical School points to a tiny culprit: the Epstein-Barr virus 1.
Epstein-Barr virus (EBV) is a herpesvirus that causes childhood infectious mononucleosis. It is sometimes referred to as the kissing disease because it is transmitted primarily through saliva and is thus associated with adolescence and the coming of love. After infection, the virus remains dormant within the B lymphocytes, the defense cells of our immune system, although in some cases it can be reactivated. The Epstein Barr virus is present in up to 95% of the population, but according to Bjorjevik’s group, in some people the infection becomes complicated and ends up developing into multiple sclerosis.
Studying whether it is possible to develop multiple sclerosis without being infected with EBV is difficult, as so many people are infected, even in early adulthood, and an unprecedented sample size is needed. U.S. military protocols enabled that nearly impossible task. All active U.S. military personnel are required to submit a blood serum sample upon entry into the military and every two years of service thereafter. Designed primarily to detect HIV, the Department of Defense Serum Repository has become a vast trove of biological samples and data comprised of more than 62 million blood samples taken from more than 10 million individuals.
The scientific team first checked whether the virus was ubiquitous among soldiers: only 5.3% of the individuals tested were not infected in their first sample. Separately, they looked for individuals who developed multiple sclerosis during their service and found 801 cases. The third question is how many of those 801 cases had tested positive for EBV: 800. 35 of those individuals had tested negative at their first donation, and all but one tested positive (a process called seroconversion) before symptoms of multiple sclerosis appeared, corresponding to a seroconversion rate of 97%. In contrast, only 57% of an initially EBV-negative control population that did not subsequently develop multiple sclerosis showed seroconversion. The median time from seroconversion to MS diagnosis was 7.5 years, with a wide range of 2 to 15 years. The proportion of Epstein Barr virus presence in persons with multiple sclerosis was 99.5%. EBV-infected persons were 32 times more likely to develop multiple sclerosis than uninfected persons.
There are always several possibilities for interpreting data like this. One possibility is that the team’s results were explained by another variable affecting the data, or reverse causality; that is, not that EBV caused multiple sclerosis, but that multiple sclerosis made it easier to be infected with EBV. To rule them out, the team performed a more detailed analysis of the serum data. Could there be another factor that simply increased the risk of getting both EBV and multiple sclerosis? The huge risk factor associated with EBV made this unlikely, but the team examined antibodies to cytomegalovirus, another saliva-borne virus that has also infected most of the world’s population, to serve as a negative control. Individuals who were negative for cytomegalovirus in their first sample did not show an increased risk of sclerosis if they later became positive for cytomegalovirus. Epstein-Barr virus did and cytomegalovirus did not.
To rule out the possibility of reverse causality, Bjornevik’s team tested 30 patients with multiple sclerosis and 30 healthy controls. They used a search tool called VirScan that can detect any antibody that targets any protein of any of the ~200 viruses known to infect humans. The only virus that showed a significantly higher presence in multiple sclerosis cases was EBV 2.
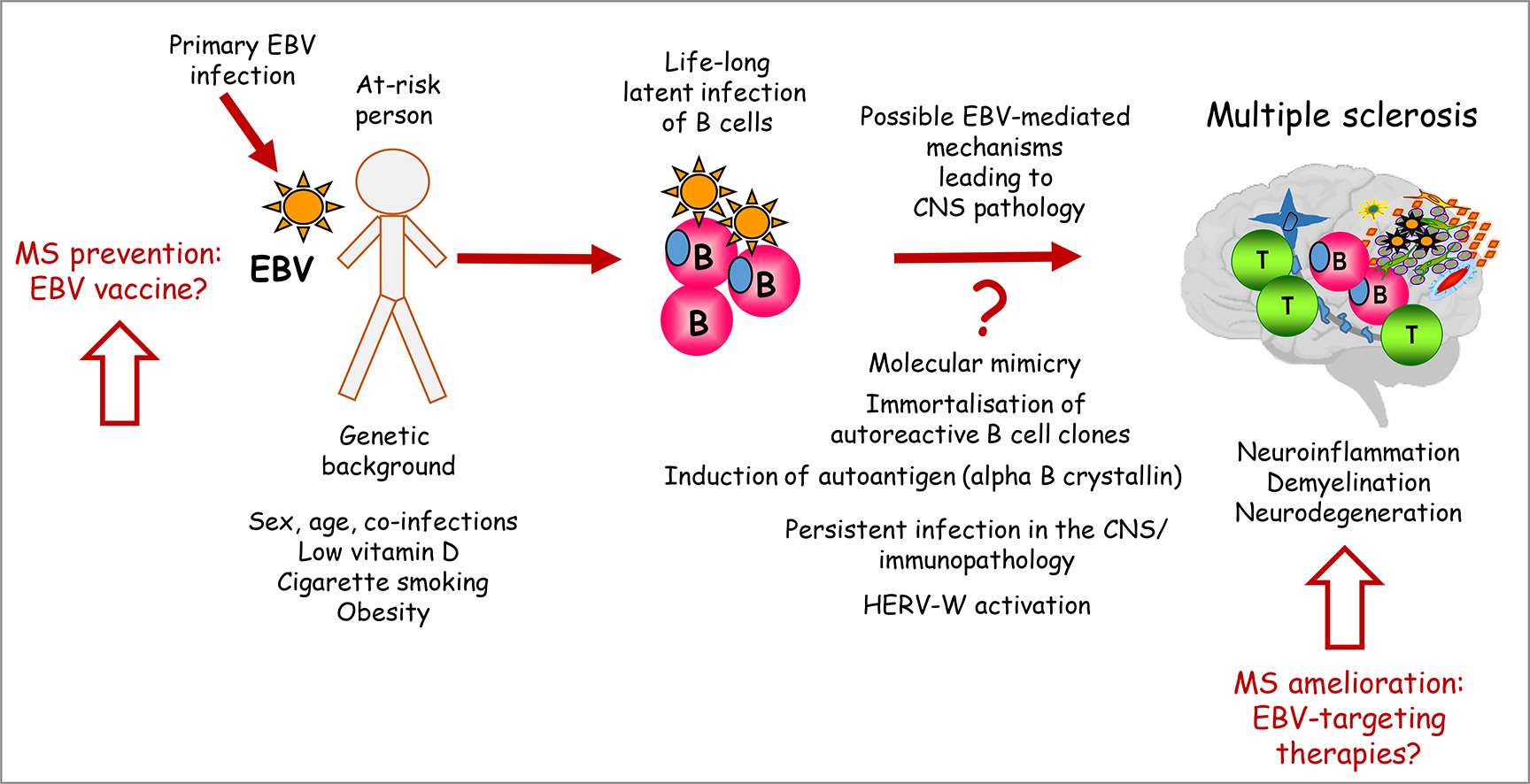
So, how does the development of multiple sclerosis work? Lanz’s group has seen that there is high-affinity molecular mimicry between a virus protein, the transcription factor EBV nuclear antigen 1 (EBNA1) and a central nervous system protein, GlialCAM, which acts as an adhesion molecule for glial cells 3. Anti-EBNA1 and anti-GlialCAM antibodies are prevalent in patients with multiple sclerosis, so in attempting to defend against the virus, the body could be attacking glial cells and causing the white matter lesions. In support of this theory, previous studies have identified EBV-infected B cells in the brains of patients with multiple sclerosis. There are other possibilities such as EBV immortalizing an autoreactive B cell line, induction of autoantigens, or prolonged infection generating an abnormal response. In any case, these results provide a mechanism for the relationship between multiple sclerosis and EBV and could guide the development of new therapies.
Epstein Barr virus may not be the only cause. EBV seropositivity is necessary to develop multiple sclerosis, but clearly not sufficient, or the disease would affect 95% of the world’s population, compared to the few million (2.8) cases of multiple sclerosis thought to exist worldwide. Genetic and environmental factors are likely to contribute to the onset of the disease, meaning that once a person has been infected with EBV, his or her genotype and phenotype will determine whether he or she will subsequently develop multiple sclerosis.
Bjornevik’s team also measured blood levels of neurofilament light chain (NfL), a biomarker of nerve degeneration. NfL levels increased in people who developed multiple sclerosis compared to those who did not. The increase occurred only after EBV infection and usually before the diagnosis of multiple sclerosis. This finding demonstrates that the nerve degeneration that accompanies sclerosis did not begin before EBV infection.
The final question raised by the Bjornevik data concerns the only EBV-negative MS patient in the study (1). The discussion section of the article identifies intersample infection or lack of seroconversion as possible explanations, but another reason may be due to diagnostic limitations. A good example is poliomyelitis, which you can diagnose as a disease caused by poliovirus or by its symptoms, acute flaccid paralysis. Before the polio vaccine, say 99% of polio cases were caused by poliovirus, but unless you define the disease based on the infectious agent, for any disease there will be occasional cases that are not caused by that agent. In fact, acute flaccid paralysis, virtually eradicated after the success of polio vaccination, is still seen in rare cases. Even if multiple sclerosis is a complication of EBV infection, when the disease is described clinically and radiologically, there will always be an occasional case that is due to something else.
The challenge now is how to develop treatments to prevent or cure multiple sclerosis. Our two fundamental strategies against viruses are vaccines and antivirals. There is currently no vaccine against multiple sclerosis, but its development is thought to be a realistic expectation. There will now be more interest when we know that it seems to be associated with a devastating disease. The most interesting therapeutic option could be adapted from immunosuppressive therapy. Currently, the most effective treatment is anti-CD20 immunotherapy (2). It is believed that what this process does is to destroy B cells, the same cells in which the Epstein Barr virus hides. Most likely, the reason anti-CD20 is so effective is because by getting rid of the cells, we also get rid of the virus, at least temporarily. A more effective treatment could target EBV directly with antivirals, leaving B lymphocytes unharmed, but these treatments do not exist either.
More on the subject:
Epstein-Barr virus linked to multiple sclerosis
References
- Bjornevik K, Cortese M, Healy BC, Kuhle J, Mina MJ, Leng Y, Elledge SJ, Niebuhr DW, Scher AI, Munger KL, Ascherio A (2022) Longitudinal analysis reveals high prevalence of Epstein-Barr Virus associated with multiple sclerosis. Science 375(6578):296-301. doi: 10.1126/science.abj8222 ↩
- Doctrow B (2022) Study suggests Epstein-Barr virus may cause multiple sclerosis. NIH Research Matters 1 February ↩
- Lanz TV, Brewer RC, Ho PP, Moon JS, Jude KM, Fernandez D, Fernandes RA, Gomez AM, Nadj GS, Bartley CM, Schubert RD, Hawes IA, Vazquez SE, Iyer M, Zuchero JB, Teegen B, Dunn JE, Lock CB, Kipp LB, Cotham VC, Ueberheide BM, Aftab BT, Anderson MS, DeRisi JL, Wilson MR, Bashford-Rogers RJM, Platten M, Garcia KC, Steinman L, Robinson WH (2022) Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Nature 603(7900): 321-327. doi: 10.1038/s41586-022-04432-7 ↩